
Rocky Mountain Health Plans
Regional Accountable Entity (RAE) Region 1
Regional Program Improvement Advisory Committee (PIAC) Meeting Agenda
Reasonable accommodations will be provided upon request for persons with disabilities. Please notify
Nicole Konkoly nicole.konkoly@rmhp.org at least one week prior to the meeting to make arrangements.
Purpose: The goals of the Regional Program Improvement Advisory Committee (PIAC) are to:
• Strengthen relationships across the region
• Share information and feedback
• Collaboratively develop solutions to critical health issues
• Prioritize our work as the RAE
When: Wednesday, September 14, 2022 from 10:00 am – 1:00 pm
Where:
• In-person at the Mesa County Workforce Center in Conference Room D, 512 29 1/2 Road, Grand
Junction, CO 81504
• Remote/virtual participation option via Zoom
Instructions to join by Zoom:
• To enter the meeting directly from web browser,
https://us06web.zoom.us/j/185525271?pwd=N0VPQnRmZXJNTDdsdld3SlYyWHd6Zz09
• To enter from https://zoom.us click “Join a Meeting” and enter Meeting ID: 185 525 271 |
Passcode: 245341
• Dial in by phone for the audio portion of the meeting (optional): 669-900-6833
Time
Topic
Topic Leader(s)
10:00 am
Welcome, Introductions and
Housekeeping
Nicole Konkoly, RMHP
10:05 am – 10:35 am
Performance Measure Updates
Jeremiah Fluke &
David Mok-Lamme,
RMHP
10:40 am – 10:55 am
Member Advisory Council Updates
Alison Sbrana, Tom
Keller & Shawn Davis
11:00 am – 11:30 am
Hospital Transformation Program
(HTP) presentation
Alison Keesler & Katie
Tiernan,
InterMountain
Healthcare
11:30 am – 12:00 pm
Lunch break

Rocky Mountain Health Plans
Regional Accountable Entity (RAE) Region 1
Regional Program Improvement Advisory Committee (PIAC) Meeting Agenda
Reasonable accommodations will be provided upon request for persons with disabilities. Please notify
Nicole Konkoly nicole.konkoly@rmhp.org at least one week prior to the meeting to make arrangements.
12:00 pm – 12:15 pm
RMHP Leadership Update:
Behavioral Health Administration
Meg Taylor, RMHP
12:15 pm – 12:55 pm
Community Reinvestment
Program Funding Ideas: Interactive
Discussion
Ivan Coziahr,
MarillacHealth & Meg
Taylor, RMHP
12:55 pm – 1:00 pm
Wrap-up / Final Comments
1:00 pm
Meeting adjourned
Next meeting: Wednesday, December 14, 2022 from 10 am – 1 pm
Rocky Mountain Health Plans (RMHP)
Regional RAE PIAC meeting minutes
Location:
Mesa County Workforce Center in Grand Junction and Zoom
Date:
Wednesday, September 14, 2022
Time:
10 am – 1 pm
Attendees –
RMHP:
Renae Anderson, Barb Bishop, Maureen Carney, Krista Cavataio, Jeremiah Fluke,
Sally Henry, Nicole Konkoly^, Cris Matoush, David Mok-Lamme, Kendra Peters, Meg
Taylor, Sarah Vaine
Attendees -
External:
Brittany Bear, Paula Belcher, Jolie Beth Boudreaux*, Mykell Christian, Janice Curtis^,
Daniel Darting, Dan Davis, Shawn Davis^, Caitlin DeCrow, Dorma Eastman, Ian Engle,
Alyssa Franklin, Shaunalee Fruit, Elaine Gerson, Noann House*^, Kris Hubbell, Terri
Hurst, Kellie Jackson*, Jessica Jensen*, Aimee Johnson, Michelle Jonjak, Alison
Keesler, Tom Keller*^, Tracy Klumker, Rochelle Larson^, Meighen Lovelace, Wade
Montgomery^, Andrea Nederveld, Rob Nelson, Hali Nurnberg^, Melissa Obuhanick,
Maria Olivo, Ashleigh Phillips, Julie Reiskin^, Allie Richmond*, Mackenzie Russo,
Melinda Sandgren, Rebecca Schickling, Cherie Schmitz, Helen Sedlar, Pam Sharratt,
Herberta Silas, Imo Succo, Katie Tiernan Johnson, Nadia Vargas
*=Voting member
^= In-person attendee
Organizations
represented:
Aspen Valley Primary Care, Axis Health System, Banner Health, Centura Health,
Colorado Blueprint to End Hunger, Colorado Criminal Justice Reform Coalition
(CCJRC), Colorado Cross-Disability Coalition (CCDC), Community Hospital, Counseling
and Education Center (CEC), DentaQuest, Family Health West, Family & Intercultural
Resource Center (FIRC) of Summit County, Grand River Health, Gunnison Valley
Health, Intermountain Healthcare, Memorial Regional Hospital, Mountain Family
Center, Mountain Family Health Centers, Northwest Colorado Center for
Independence, Pagosa Springs Medical Center, PDF Consulting, Primary Care
Partners, Quality Health Network (QHN), ReVision ADHD, Southwest Health System,
Summit County DHS, St. Anthony Summit Hospital, Southwest Colorado Area Health
Education Center (SWCAHEC), University of Colorado School of Medicine, Valley View
Hospital
2
Agenda Items
1. Call to Order: Nicole Konkoly, RMHP RAE Network Relations Manager, called the meeting to order
at approximately 10 am and participants introduced themselves in the room and via the chat
feature on Zoom. Nicole shared the goals of the PIAC, which are to:
• Strengthen relationships across the region
• Share information and feedback
• Collaboratively develop solutions to critical health issues
• Prioritize our work as the RAE
2. Performance Measurement Updates – David Mok-Lamme, RMHP
We received constructive feedback about the way we’ve been doing these presentations. We’ll
be slowing down to talk about what exactly is included in each of the measures instead of moving
quickly through all the measures (there are a lot!). We’ll leave space for participants to share
their own thoughts, both from themselves and the communities and organizations they represent,
about their experiences and recommendations for improving the healthcare delivery system.
Today, we’ll be doing a deep dive on 2 different measures, all of which are part of the Behavioral
Health Incentive Program (BHIP), which are statewide measures established by the Department of
Health Care Policy and Financing (HCPF).
• Substance Use Disorder (SUD) Engagement – measure starts when a member first
receives a service for SUD, which could take place in an outpatient, detox or
residential setting. To meet the measure, the member must receive two follow-up
services within 30 days. Services can include therapy, evaluation and management
services provided by a physician or physician’s assistant, or community services such as
assertive community treatment. Our performance has remained relatively flat at
around 47%; we’ve improved but are short of our target which is set at 49%.
• Mental Health Inpatient Follow-up – looks at follow-up services after mental health
psychiatric inpatient stays. One visit needs to occur within 7 days to meet the
measure. We were doing better on the measure in July 2020 (49%). We’ve been
hovering around 45% more recently. The set of services that members can receive
within that 7-day time-period are the same as the SUD Engagement measure.
Comments & Questions:
• Why are peer services excluded? Should all peer services count in the measures? The state has
distinguished peer services by high-intensity – e.g. assertive community treatment and low
intensity – e.g. targeted case management, drop-in centers. Only a percentage of the services
that peers provide – i.e. high-intensity services - are included in the measures at this time.
• If someone is discharged on psych meds, are we looking at whether they’re connected with a
psychiatrist who can monitor their medications? Medication management services must be
provided by a provider who can prescribe medications.
• Patient education is critical. For example, are patients who are discharged on psych meds
educated that they need to get laboratory follow-up? It’s supposed to happen as part of
discharge planning and there are efforts to improve it but that’s outside the scope of these
3
particular measures. Patients should be treated with dignity and be empowered to understand
and assume responsibility for follow-up care. Perhaps peers could give out a handout when
someone is discharged.
• The BHIPs miss the component of understanding member experience and what patients
experience beyond the actual visits. They’re narrow output-type measures. There are broader
discussions happening with both HCPF and the Behavioral Health Administration (BHA) to
discuss expanding the measures. People who are interested in joining these
discussions/workgroups can contact David or Meg for details. RMHP has been advocating for a
more comprehensive set of measures that include the member voice/perspective.
• More stringent measures should be put in place on the front end to ensure that members are
getting the support they need in a timely manner with a competent provider. More
accountability measures such as a more precise feedback loop between providers and the
RAEs so that the RAE knows quickly whether a member is getting the care they need.
•
Can vouchers be used for providers that don’t take Medicaid? Especially in rural areas, this
can be a challenge. The Single Case Agreement process can be arduous for providers. It’s
difficult for the RAEs to work outside of the administrative infrastructure that we have.
Members are encouraged to contact us about specific providers that they’re wanting to see
and/or that are struggling with the Single Case Agreement process or Medicaid enrollment
process, and we can help troubleshoot them on a case-by-case basis.
• What process can stakeholders use to give RMHP input on measure recommendations?
o Ian Engle and Tom Keller are voting members on the ACC PIAC and can take
recommendations to that committee.
o It’s RMHP’s responsibility to listen to what participants share at these meetings and
communicate them to HCPF. For example, we can share with HCPF that our PIAC
strongly recommends that all peer services be included in the BHIPs.
o ACC PIAC subcommittees are also forums where the Key Performance Indicators (KPIs)
and BHIPs are discussed, and recommendations are made to the ACC PIAC.
Strategies RMHP is using to improve the member experience and access to quality care:
• RMHP has several care coordinators who focus on transitions of care and discharge planning
who help ensure timely follow-up care. Our hope is by building trusted relationships,
members know who to contact if they’re not getting the follow-up care they need.
• We’re also broadening the behavioral health organizations that we’re partnering with to
provide that timely quality care for members. This includes being more actively involved in
helping members get access to care and broadening the provider network that we’re working
with for follow-up visits. Historically, we only shared BHIP incentive funding with CMHCs.
Starting in July 2022, we are sharing funding with a broader group of providers, based on how
they provide timely follow-up care.
3. Member Advisory Council updates
Larimer County Member Advisory Council
4
Alison Sbrana shared that following are the primary topics that have been discussed by the council
over the past several months:
• Pain Management – members are reporting barriers to finding providers who will see them if
they are already taking opioids as well as finding providers who will prescribe opioids if they
have an appropriate need for them. Ideas to address these barriers include HCPF providing
educational initiatives that shares the patient perspective and RMHP recognizing providers
that prescribe opioids appropriately and possibly assemble a panel discussion to teach other
providers how to do this. There are also some issues with the physical therapy benefit
limitations. People like me may not get better with physical therapy but if we don’t receive
it, we will need to access much more acute/expensive levels of care such as repeat
emergency visits or hospitalizations.
• Behavioral Health Access – People with developmental disabilities and people with complex
medical needs have a very difficult time receiving appropriate inpatient psychiatric care. We
are going to have a new behavioral health facility in Larimer County but there are concerns
that this population will not be adequately addressed and there are also concerns that the
length of stay in the new facility will not be adequate. We want to see appropriate cultural
competency among the staff of the facility. We’ve been meeting regularly with the director
of the new facility to share feedback and ideas.
Spanish Speaking Member Advisory Council
Shawn Davis shared that the Colorado Cross-Disability Coalition (CCDC) is hiring a person who will be
responsible for facilitating the Spanish Speaking Member Advisory Council as well as advocacy for
helping families navigate the healthcare system. We will share the job description as part of the
meeting material packet. If anyone knows of someone who may be interested, please share the
information, and encourage them to apply. The goal is to have the council up and running before the
end of the year.
West Slope Member Advisory Council
Tom Keller shared that the council last met on Monday. Jose Chavez came and talked about the
community building and health equity organizing work that’s been happening in the Clifton
community in Mesa County. A lot of work is being done to engage with the Tribes. The group will be
reviewing some newly updated member materials. A Request for Proposals (RFP) for case
management agencies will be going out soon, and HCPF has identified some pillars about what case
management redesign should look like. The group discussed what the following terms mean and look
like: Accountability; Simplicity; Integrity; and Transparency.
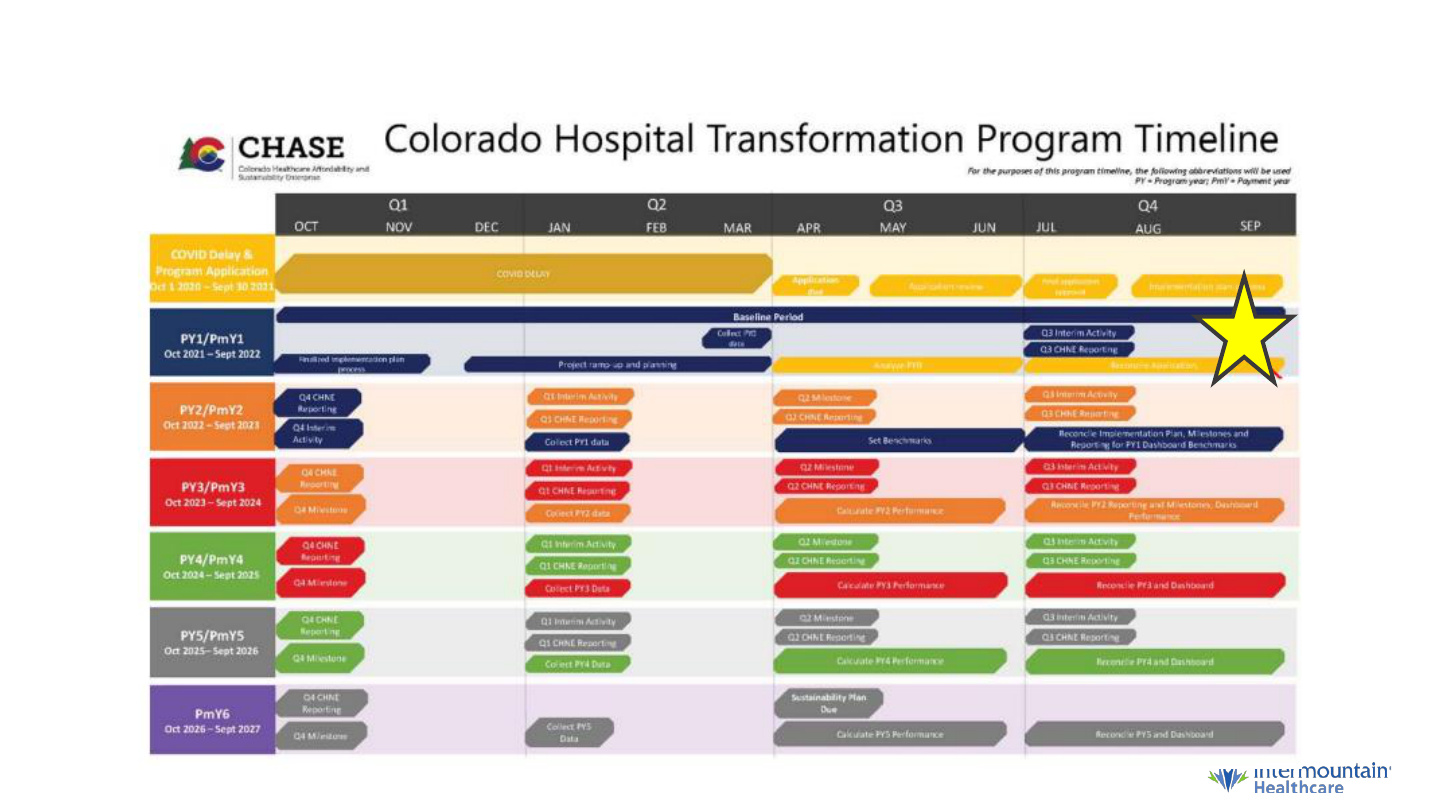
4. Hospital Transformation Program (HTP) Community Engagement presentation from
Intermountain Health Care
Barb Bishop, Clinical Program Manager with RMHP, introduced Alison Keesler, Program Manager,
Network and Risk Programs and Katie Tiernan, Executive Director, Community Impact who gave a
presentation on the Hospital Transformation Program at Intermountain Healthcare.
SCL Health merged with Intermountain Healthcare in April 2022. SCL Health was a nonprofit
healthcare system founded by the Sisters of Charity of Leavenworth that opened their first hospital
5
in Colorado in 1873. Intermountain Healthcare is also a nonprofit healthcare system, headquartered
in Salt Lake City and nationally recognized for innovation in access to care and value-based care. SCL
Health’s executive leadership was retained post-merger and the Boards of Directors continue to have
oversight and authority. Retaining local governance of our Colorado hospitals allows us to respond to
community needs in an appropriate way. Operate 5 hospitals in Colorado, including St. Mary’s
Hospital in Grand Junction.
The overall objective of the Hospital Transformation Program (HTP) is to move away from paying for
volume and into paying for value.
For St. Mary’s Hospital and all other Intermountain hospitals, the following measures have been
selected; some were mandated by the state, and some were selected by the hospital.
• Adult 30-day all-cause risk adjusted readmission rate
• Percentage of patients with ischemic stroke who are discharged on statin medication
• Social determinants of health screening and RAE notification
• Screening for transitions of care supports in adults with disabilities
• Screening and referral for perinatal depression and anxiety and notification of positive
screens to the RAE
• Collaboratively develop and implement a mutually agreed upon discharge planning and
notification process with the appropriate RAEs for eligible patients with a diagnosis of mental
illness or substance use disorder (SUD) discharged from the hospital or emergency department
• Using alternatives to opioids (ALTO’s) in hospital Emergency Departments – decrease opioid
use and increase use of ALTO
• Hospital Index
• Implementation/expansion of telemedicine visits
• Severity Adjusted Length of Stay
Comments & Questions:
• Appreciate that the length of stay measure is looking at people being discharged prematurely
and not focusing solely on people staying too long. Not getting enough care leads people to
re-enter the system; so it’s important to find the right balance.
• Opioid alternatives/ALTOs – need to be mindful of consumer choice and quality of care. It’s
important to ensure that ALTOs are used at safe and appropriate times. When people who
have chronic pain and other complex medical needs don’t receive appropriate care in the
outpatient setting, they wind up in the Emergency Department. Katie & Alison will bring this
feedback to the ALTO committee. Perhaps the Colorado Hospital Association can provide
recommendations for pain management in the ambulatory setting.
• There’s a lot of focus on screenings. Screenings can make people feel like a lab rate or some
type of specimen. That person needs to be meaningfully engaged, and not treated as a
passive observer. How is screening done in a way that builds trusted relationships, rather than
being run through a gauntlet of gatekeepers? Initial screenings are done by nurses. They ask
questions to find out about communication preferences, transition of care and social
determinants of health needs. If a patient screens positive, they are referred to a Care
Manager, and the RAE is notified which domains the person screened positive for and the
resources to which they were referred. This allows the RAEs to follow-up with the person to
determine if they received the appropriate resources. Banner Health is working on sharing
screening data between their hospital facilities and primary care clinics so that a patient isn’t

6
having to answer the same questions each time they have a visit. They are also working on
solutions to allow patients to fill out screenings prior to their visit. Grand River Health is not
just screening for social determinants of health, but connecting patients to resources and
make sure they receive follow-up. They use the Community Resource Network (CRN) through
Quality Health Network (QHN) that helps connect patients to resources. The data collected
through the HTP will allow us to see where the highest needs exist, as well as where the
biggest gaps in resources exist. This data can be taken to legislators and community benefit
departments when requesting funding.
• Stain medications – every patient that presents with ischemic stroke are discharged on statin
medication. A participant expressed concern about consumer choice. The stroke measure is
also based on the patient’s LDL and patients do have a choice to decline.
InterMountain Healthcare will take all of participants’ feedback back to the HTP Implementation
Team.
“Caring for Community” annual forum will take place on Tuesday, November 15
th
at 5 pm. To be
added to the invitation list, contact Samantha.m[email protected]
5. Lunch Break (15 minutes)
6. RMHP Leadership Update: Behavioral Health Administration – Meg Taylor, RMHP
Meg shared her understanding of where this stands at the current time. The Behavioral Health
Administration (BHA) was formed through legislation as a new entity that essentially replaced what
was previously known as the Office of Behavioral Health (OBH). While a few functions remain under
OBH, the majority of functions have transitioned. Our crisis services contract, for example, is now
with the BHA. Managed Service Organization (MSO) contracts are also under the BHA. Contracts that
the state holds with Community Mental Health Centers (CMHCs) are also under the BHA. In Spring
2023, the state will release a Request for Proposals (RFP) for new entities called Behavioral Health
Administrative Services Organizations (BHASOs). BHASOs will go live July 1, 2024. The BHASOs will be
responsible for the following functions: crisis services, MSO services, state contracts with CMHCs, as
well as a huge component of care coordination and care navigation. This is for all residents of
Colorado, but people who have Medicaid as their health plan will still receive many services through
the RAEs. There will be an advisory council for the BHASOs, similar to the RAE PIACs. It’s not yet
been determined what this will look like regionally, however there’s speculation that the BHASO
regions will align with the RAE regions. RMHP is currently in this space and would like to continue
working in this space under the new model.
7. Community Reinvestment Program Funding Ideas: Interactive Discussion
Meg thanked the PIAC voting members who met between now and the last PIAC meeting to identify
potential uses for community investment funding. RMHP earmarked $500,000 of community
investment funding for the PIAC to help us determine where to invest this funding in the community.
Parameters for funding: the funding cannot be used for Medicaid-funded services or services that are
available through existing funding streams such as Long-Term Services and Supports (LTSS) waivers.
An example is Southwest Center for Independence received funding from RMHP to provide
transportation services to help people achieve freedom from isolation such as rides to visit family
and friends, participate in recreational activities, etc. These services are not covered under the
Medicaid Non-Emergent Medical Transportation benefit.
7
The funding will renew each year, but changes can be made as necessary. For example, if we’re at
mid-year and not seeing the results we were expecting, we can make adjustments. Although funding
is dependent on our membership and performance on the quality measures, we will do our very best
to keep the funding consistent from year to year.
The top ideas that came out of the voting member brainstorming session are the following:
• Social determinants of health community benefit fund: This fund would cover anything that
Medicaid does not cover, such as rental assistance, tuition assistance, car seats, etc. The
person who presented the idea used an example of a homeless individual that their
organization could only temporarily house them, but if they could have helped the person get
stabilized in short-term housing, they could really help fill the gaps but there was no funding
available.
• Navigators for SSDI and SSI applications: There is currently a wait list of people who need
application assistance, and applications can take 40 hours. The wait time for SSI and SSDI
application processing is inhumanely long, and less than 30% of applications are approved the
first time. The denial appeal process can take 1 to 2 years, during which they’re advised not
to work. This population is extremely vulnerable, especially during the application processing
timeline. The idea is to provide dedicated funding for individuals who are knowledgeable
about the application process to help increase the likelihood of application approval so that
they can be connected to benefits sooner. We’ll need to engage with the counties as part of
this work. Provider support could be a component of this model: how can providers help
someone navigate the application process? CCDC offered a training on this specific topic to
RMHP providers, and this could be offered again. A network for cross-training on best
practices would be helpful. It will be very important to document and capture what we’re
doing so that it can be replicated; this model could likely be replicated by other
RAEs/organizations. The model could not only be replicated statewide, but nationally.
Participants suggested the following additional ideas:
• Set up a small study to see what outcomes could be achieved by educating a group of people
with Type 2 diabetes, while also providing them with a set amount of funding to spend on
organic, whole foods as well as a continuous glucose monitor, and ongoing support and
education. The same process could also impact many members who have chronic health
issues.
• A community health worker model to support people with Long COVID
• In a lot of our communities, two of the major issues affecting the health and wellbeing of
people with disabilities are:
o Housing – home modifications are one way we can help people live safely in their
homes
o Personal attendant services – with workforce shortages and salary limitations, it’s very
challenging to hire personal attendants
Next steps: Voting members will take information from today’s discussion into consideration, and
submit their proposals to RMHP. An update will be provided at the December meeting.
8
Action items:
• If the SSI/SSDI application navigation proposal is approved by voting members, Julie Reiskin,
Ian Engle, Alison Sbrana and Hallie Nurnberg will form a workgroup to help get the project off
the ground.
• RMHP will send an updated calendar invite for the December meeting. It was originally
scheduled for Wednesday, December 14
th
but will now be held on Tuesday, December 6
th
so
that it coincides with the West Slope Member Advisory Council meeting that will take place on
Monday, December 5
th
.
• RMHP is organizing a photo shoot for Members to be used in materials that highlight the
diversity and value of Medicaid. A HCPF video campaign was recently implemented for this
same purpose.
Next meeting: Tuesday, December 6, 2022, from 10 am – 1 pm via a hybrid format. In-person
location will be at the Mesa County Workforce Center.

The Hospital Transformation
Program at Intermountain
Healthcare
Alison Keesler, MHSA
Program Manager, Network and Risk Programs
Katie Tiernan
Executive Director, Community Impact

Agenda
ASK
Seek to
understand
Hospital
Transformation
Program (HTP)
Seek to
understand
community
engagement
requirements
Provide
feedback on
interventions

Mission for our Catholic entities: “We reveal and foster God's healing
love by improving the health of the people and communities we serve,
especially those who are poor and vulnerable.”

Hospital Transformation Program (HTP)
• Five-year State-mandated Colorado hospital down-side risk program
• CHASE Board provides program oversight and provider fee management
• Cost and Quality measure performance to gain provider fee dollars
• Provider fee dollars: a collection of dollars paid by hospitals, federally matched, then
redistributed back to hospitals based on their volume of undercompensated care
• HTP goals are to improve quality outcomes through measure performance and
decrease cost to the State
• HTP Community Advisory Committee reports to the State
Program Timeline

Measures
SW-RAH1
Adult 30-day all-cause risk adjusted readmission rate
RAH4
Percentage of patients with ischemic stroke who are discharged on statin medication (eCQM)
SW-CP1
Social Determinants of Health screening and RAE notification
CP4
Screening for transitions of care supports in adults with disabilities
CP6
Screening and referral for perinatal depression and anxiety and notification of positive screens to the RAE
SW-BH1
Collaboratively develop and implement a mutually agreed upon discharge planning and notification process with the appropriate RAE's for
eligible patients with a diagnosis of mental illness or substance use disorder (SUD) discharged from the hospital or emergency department
SW-BH3
Using Alternatives to Opioids (ALTO's) in hospital ED's – Decrease opioid use and increase use of ALTO
SW-COE1
Hospital Index
COE2
Implementation/expansion of telemedicine visits
SW-PH1
Severity Adjusted Length of Stay

Measure Work
Required
Measures
Reduce
readmissions
Ask about social
needs (housing,
food,
transportation,
utilities, violence)
Provide good
discharge plans for
people with
behavioral health
concerns
Give non-opioid
pain medications to
people in the
Emergency
Department
(ALTOs or
ALTernatives to
Opioids)
Fewer
complications in
medical care
Reduce the length
of stay for patients

Measure Work Continued
Reduce avoidable
hospital use
Focus on core
populations (people
with identified
needs such as
pregnancy and
chronic conditions
such as diabetes)
Help people with
behavioral
health/substance
use disorders
Provide efficient
care
Improve population
health/total cost of
care

Community Health Neighborhood Engagement (CHNE)

• Hospital Community Benefit
engages with community year-
round to identify and connect
community needs with initiative
planning
• “Caring for Community” annual
forums
• 5 p.m. on November 15, 2022
• Email Samantha McCrory,
Community Impact
Coordinator, to be added to
invitation list:
CHNE at Intermountain

Questions?

Proprietary information of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.
Community Investment
6
• SDOH Slush Fund
• Integrated School Health Home
• Language Justice
• Telehealth Services in Preferred Language
• ReSet O Technology App
• Navigators for SSDI and SSI Applications
• Education about Legal Status

