
1549
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
Members of the American Academy of Sleep Medicine developed consensus recommendations for the amount of sleep needed to promote optimal health
in children and adolescents using a modied RAND Appropriateness Method. After review of 864 published articles, the following sleep durations are
recommended: Infants 4 months to 12 months should sleep 12 to 16 hours per 24 hours (including naps) on a regular basis to promote optimal health.
Children 1 to 2 years of age should sleep 11 to 14 hours per 24 hours (including naps) on a regular basis to promote optimal health. Children 3 to 5 years
of age should sleep 10 to 13 hours per 24 hours (including naps) on a regular basis to promote optimal health. Children 6 to 12 years of age should sleep
9 to 12 hours per 24 hours on a regular basis to promote optimal health. Teenagers 13 to 18 years of age should sleep 8 to 10 hours per 24 hours on a
regular basis to promote optimal health. Sleeping the number of recommended hours on a regular basis is associated with better health outcomes including:
improved attention, behavior, learning, memory, emotional regulation, quality of life, and mental and physical health. Regularly sleeping fewer than the
number of recommended hours is associated with attention, behavior, and learning problems. Insufcient sleep also increases the risk of accidents, injuries,
hypertension, obesity, diabetes, and depression. Insufcient sleep in teenagers is associated with increased risk of self-harm, suicidal thoughts, and
suicide attempts.
Commentary: A commentary on this article apears in this issue on page 1439.
Keywords: pediatric, sleep duration, consensus
Citation: Paruthi S, Brooks LJ, D’Ambrosio C, Hall WA, Kotagal S, Lloyd RM, Malow BA, Maski K, Nichols C, Quan SF, Rosen CL, Troester MM, Wise MS.
Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: methodology and discussion.
J Clin Sleep Med 2016;12(11):1549–1561.
1.0 INTRODUCTION
Healthy sleep requires adequate duration, appropriate timing,
good quality, regularity, and the absence of disturbances and
disorders. Sleep duration is a frequently investigated sleep
measure in relation to health outcomes. Many studies have
shown that adequate sleep duration is associated with better
attention, behavior, cognitive functioning, emotional regula-
tion, and physical health among children.
1–3
A panel of 13 experts in sleep medicine and research used a
modied RAND Appropriateness Method
4
to develop recom-
mendations regarding the sleep duration range that promotes
optimal health in children aged 0–18 years. The Consensus
Recommendations
5
were previously published, and this report
expands on the methodology, results of the literature search,
key ndings from published research, overview of discus-
sion by the panel members during the in-person meeting, and
limitations of the process to answer the critical question: How
much sleep is needed for optimal health in children?
SPECIAL ARTICLES
Consensus Statement of the American Academy of Sleep Medicine
on the Recommended Amount of Sleep for Healthy Children:
Methodology and Discussion
Shalini Paruthi, MD, Moderator
1
; Lee J. Brooks, MD
2,3
; Carolyn D’Ambrosio, MD
4
; Wendy A. Hall, PhD, RN
5
; Suresh Kotagal, MD
6
; Robin M. Lloyd, MD
6
;
Beth A. Malow, MD, MS
7
; Kiran Maski, MD
8
; Cynthia Nichols, PhD
9
; Stuart F. Quan, MD
10
; Carol L. Rosen, MD
11
; Matthew M. Troester, DO
12
;
Merrill S. Wise, MD
13
1
Saint Louis University, St. Louis, MO;
2
Children’s Hospital of Philadelphia, Philadelphia, PA;
3
Liaison for the American Academy of Pediatrics;
4
Brigham & Women’s Hospital,
Boston, MA;
5
University of British Columbia School of Nursing, Vancouver, BC;
6
Mayo Clinic, Rochester, MN;
7
Vanderbilt University Medical Center, Nashville, TN;
8
Boston
Children’s Hospital, Boston, MA;
9
Munson Sleep Disorders Center, Traverse City, MI;
10
Harvard Medical School, Boston, MA;
11
Rainbow Babies & Children’s Hospital, Cleveland,
OH;
12
Barrow Neurologic Institute at Phoenix Children’s Hospital, Phoenix, AZ;
13
Methodist Healthcare Sleep Disorders Center, Memphis, TN
pii: jc-00365-16 http://dx.doi.org/10.5664/jcsm.6288
2.0 METHODS
The American Academy of Sleep Medicine (AASM) Sleep
Duration Consensus Conference used a modied RAND Ap-
propriateness Method (RAM)
4
to establish consensus for the
amount of sleep needed to promote optimal health in children
and teenagers.
2.1 Expert Panel Selection
In accordance with the recommendations of the RAM, the Sleep
Duration Consensus Conference panel comprised 13 voting
members, including a moderator. All panel members are experts
in sleep medicine and/or sleep science. The panel members were
recommended by the Board of Directors of the AASM.
Panel members were sent a formal letter of invitation from
the AASM and were required to complete Conict of Interest
disclosures before being ofcially accepted. To avoid further
conicts, panel members were not permitted to participate in
similar consensus activities by other organizations.
1550
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
2.2 Modified RAND Appropriateness Method
The RAND Appropriateness Method uses a detailed search
of the relevant scientic literature, followed by two rounds
of anonymous voting to determine consensus on the appro-
priateness of a recommendation. The rst round of voting is
completed without panel interaction to prevent panel members
from inuencing each other’s votes. The second round of vot-
ing occurs after a panel discussion of the available evidence
and Round 1 voting results.
In a modication to RA M, the Consensus Conference included
a third round of voting, which considered all available evidence
and the previous voting results, to establish a single recommen-
dation for the amount of sleep needed to promote optimal health
for each age group in children. The third round also involved a
discussion of the merits of recommending an optimal sleep dura-
tion range versus a simple threshold value. The nal Consensus
Recommendations resulted from the third round of voting.
The charge to the Consensus Conference panel was to de-
termine a sleep duration recommendation for healthy children.
Panel members voted on the appropriateness of one-hour in-
crements ranging from < 6 to ≥ 18 hours of sleep. One-hour
increments were selected because these were the most com-
monly reported units in epidemiologic and experimental stud-
ies. Substantial heterogeneity was present in the sleep duration
assessment instruments. The consensus recommendations
focused on overnight and daytime nap durations when appro-
priate as napping is considered biologically normal under the
age of 7 years. The nal recommendations were based on the
one-hour values that were determined by the panel to be “ap-
propriate” to promote optimal health in children.
2.3 Detailed Literature Search and Review
The AASM Board of Directors charged the panel with devel-
oping a recommendation for sleep duration in healthy children.
This charge coincides with the goals of the National Healthy
Sleep Awareness Project (NHSAP) and with the Sleep Health
Objective of Healthy People 2020 to “increase the proportion
of students in grades 9 to 12 who get sufcient sleep.”
6
The scope of the recommendation was limited to children
aged 0–18 years. After a preliminary review of the litera-
ture, prior Centers for Disease Control and Prevention (CDC),
AASM, and National Sleep Foundation (NSF) recommenda-
tions, as well as commonly frequented websites, the following
age groups were created: < 12 months, 12 months to < 3 years,
3 years to < 6 years, 6 years to < 13 years, and 13–18 years.
There was substantial overlap of age groups within the litera-
ture, and this was discussed during the in-person conference.
A preliminary search of the literature and specic National
Library of Medicine Medical Subject Headings (MeSH) terms
identied several health outcomes that were most commonly
examined in relation to sleep duration in children. Based on
this evidence, the panel decided to focus on the relationships
between sleep duration and the following 10 health categories:
cardiovascular health, developmental health, human perfor-
mance, general health, immunology, longevity, mental health,
metabolic health, pain, and cancer.
After establishing the health categories, a detailed literature
search was performed in PubMed on October 1, 2015. The
search terms used for the literature search are detailed in the
supplemental material. The search was restricted to studies in
human children ages 0–18 years, published in English, with no
publication date limit. Case reports, editorials, commentaries,
letters and news articles were excluded from the search results.
The initial search produced 1,040 publications. The search re-
sults were reviewed based on title and excluded a priori for
the following reasons: focus on sleep quality or fatigue instead
of sleep duration, assessing sleep duration in specic disor-
ders or sleep disorders, experiments on total sleep deprivation,
children sleeping outside normal day/night sleep schedules, as-
sessments of sleep deprivation as a treatment (insomnia or de-
pression), and focusing on medication effects on sleep duration.
Application of these restrictions resulted in 864 publications.
The panel reviewed the abstracts of these remaining publi-
cations using the criteria described above. Citation pearl grow-
ing was used to capture additional important publications that
were not identied by the search. Accepted publications were
graded for quality using the Oxford criteria.
7
All accepted pub-
lications were reviewed in detail and the data listed in Table 1
were extracted.
Based on the data extraction, accepted studies were subdi-
vided into the categories listed in Table 2.
The extraction sheet and full text of all accepted publica-
tions were made available to the panel members for review.
Each panel member was assigned to a particular health domain
and asked to identify the most informative studies based on
study design and evidence quality. After review of the litera-
ture, the domains of pain and cancer did not contain sufcient
data to guide sleep duration recommendations and therefore
were excluded prior to Round 1 Voting. After lengthy discus-
sion at the conference, the domain of longevity was excluded
prior to Round 2 Voting. A second PubMed literature search
Table 1—Data extracted from studies for evidence tables.
1 Study design
2 Oxford grade
3 Number of study participants
4 % of female participants
5 Method by which sleep duration was obtained
6 Age range of child participants
7 Major outcomes and conclusions
Table 2—Health domains.
1 Cardiovascular health
2 Developmental health
3 Human performance
4 General health
5 Immunology
6 Longevity
7 Mental health
8 Metabolic health
9 Cancer
10 Pain

1551
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
was performed during the conference on February 19, 2016 to
collect more recent relevant studies.
2.4 Round 1 Voting
Prior to the conference, panel members reviewed the accepted
publications and extraction sheets. Based on their review of
this material and their clinical and research expertise, mem-
bers voted to indicate their agreement with the following state-
ment, “Based on the available evidence, [x] hours of sleep is
associated with optimal health within the [x] category in the
[x] age group.” “Hours of sleep” was categorized as: < 6 hours,
6 to < 7 hours, 7 to < 8 hours, 8 to < 9 hours, 9 to < 10 hours,
10 to < 11 hours, 11 to < 12 hours, 12 to < 13 hours, 13 to < 14
hours, 14 to < 15 hours, 15 to < 16 hours, 16 to < 17 hours,
17 to < 18 hours, ≥ 18 hours. The panel members voted us-
ing a 9-point Likert scale, where 1 meant “strongly disagree,”
9 meant “strongly agree,” and 5 meant “neither disagree nor
agree.” Panel median values were placed into three broader
categories, with the following interpretations: 1–3 indicated
disagreement with the statement, 4–6 indicated uncertainty,
and 7–9 indicated agreement with the statement.
Panel members were instructed not to discuss the evidence
or their votes with each other to ensure independence. Panel
members’ votes were collected by email and compiled to
determine the median and distribution of votes. Individual
results tables were created and distributed to the members
at the consensus conference, displaying the distribution of
votes (anonymously), the member’s vote, and the median vote
(Figure 1).
2.5 Conference Proceedings and Round 2 Voting
Prior to the conference, panel members were selected to be-
come domain experts for each domain. At the conference,
members reviewed the results of Round 1 voting for a domain,
and then the domain experts presented a review of the best
available evidence for that domain. Panel members then dis-
cussed the results of Round 1 voting, the accepted publica-
tions for the domain and any other relevant evidence. After
discussion, panel members completed Round 2 voting for the
age groups within the domain, following the same procedures
from Round 1 voting. The conference proceeded in this man-
ner for each domain.
2.6 Round 3 Voting and Development of
Recommendations
Panel members reviewed and discussed Round 2 voting results
for all domains and the entire body of accepted publications
in preparation of voting on recommendation statements. After
Figure 1—Round 1 voting results.
Round 1 voting was based on voting across all age groups under the following eight domains: cardiovascular health, developmental health, human
performance, general health, immunology, longevity, mental health and metabolic health.

1552
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
discussions concluded, panel members completed Round 3
voting for a single recommendation of appropriate sleep dura-
tion range for each age group, following the same procedure as
for Round 1 and Round 2 voting, but with the following state-
ment: “Based on the available evidence, [x] hours of sleep is
associated with optimal health in [x] age group.”
Based on the results of Round 1 and Round 2 voting, the
conference discussions, and with the agreement of all the panel
members, the infant (0 to 12 months) category was reduced to 4
to 12 months. This decision was based on the lack of evidence
in this 0–4 month old age group. Thus, no recommendations
were made for children under 4 months of age for any of the
categories.
Upon completion of Round 3 voting, the panel members
reviewed the voting results and developed the recommenda-
tions. The age groups and hour ranges were simplied to those
presented in the consensus statements for the purposes of
simplifying recommendations and ensuring clarity.
The nal recommendations were submitted to the AASM,
Sleep Research Society (SRS), American Academy of Pediat-
rics (AAP), and American Association of Sleep Technologists
(AAST) Boards of Directors for their endorsements.
3.0 SUMMARY OF LITERATURE
The following sections summarize the key evidence consid-
ered by the panel in developing the recommendations while
acknowledging that a complete evaluation of the evidence is
beyond the scope of this consensus process.
For each domain, the panel reviewed studies with children
from all over the world, addressing sleep duration and health
outcomes across the prespecied age ranges. Within each do-
main, there were topics without information for some of the age
groups, and often studies spanned several of our prespecied
age groups. Studies that assessed the relationship between
sleep duration and the search term of interest were the most
informative. Many studies reported more than one outcome.
However, emphasis was placed on longitudinal or cross-sec-
tional cohort studies that reported sleep duration in unselected
general populations as well as smaller studies of unconstrained
sleep in healthy children. Some studies only provided correla-
tion or regression coefcients and thus were minimally infor-
mative. Others reported the association between general health
and sleep duration, but only at a limited number of thresholds.
In most studies, sleep duration was assessed by parent or child
self-report. Polysomnographic data and actigraphy were con-
sidered when appropriate such as in studies of unconstrained
sleep in the laboratory or at home. Systematic comparisons be-
tween studies were challenging and in most cases not possible.
The following domains and information were reviewed.
3.1 General Health
In the general health domain, the number of children in each
study ranged from less than 25 to over 74,000.
Within the 4-months to < 12 months age range, there were
few studies. However, two large prospective birth cohorts
indicated that over a 24-hour period, healthy infants slept
slightly > 13 to slightly > 14 hours.
8,9
Furthermore, infants
sleeping for lesser amounts of time had a greater likelihood of
quality of life issues later in childhood.
9
For children in the 1 to < 3 years and 3 to < 6 years age
ranges, there were only a small number of studies to review.
One cohort study reported sleep durations between 11 and
12 hours in normal children.
8
Limited data also suggested
that sleeping less than 10 hours was associated with a greater
risk of accidental injury
10
and reduced quality of life several
years later.
11
More studies were available that addressed general health
outcomes in older children including those with polysomno-
graphic data during unconstrained sleep.
12,13
In the 6 to < 13
years age group, the panel observed that this was a period of
rapid physical and mental development with more sleep appro-
priate for children at the lower end and less sleep for those at
the higher end of the age range. Most informative was a large
meta-analysis of children from 20 countries that indicated
children between 9 and 12 years of age slept approximately 10
hours per night.
14
In addition, data were available suggesting
children sleeping 10 hours or more per night reported better
health.
15
In the 13–18 year age range, increased rates of injury
were noted for those sleeping less than 7 or 8 hours
16,17
and
better health was reported for those sleeping 9 hours or more.
15
A meta-analysis found that in teenagers, sleep declined con-
tinuously from between 9 and 10 hours at age 13 to between
slightly less than 8 to slightly greater than 9 hours at age 18
years of age.
15
Extended sleep duration was noted on weekends
compared with weekdays.
In summary, limited information indicates that there is a
continuous decline in the amount of sleep required for nor-
mal general health. Lesser amounts are associated with poorer
overall health and reduced quality of life later in childhood.
However, there is little information regarding any impact of
excessive sleep on overall health.
3.2 Cardiovascular Health
Many of the studies in the cardiovascular domain examined
the relationship between sleep duration and hypertension. Oth-
ers looked at body mass index, waist circumference, serum lip-
ids, C-reactive protein (CRP), and hemoglobin A1C (HbA1C).
Most studies were cross-sectional, observational, retrospec-
tive or cohort design; none were randomized controlled stud-
ies. The number of participants varied from as few as 20 to
just over 5,500. No studies in this domain included children
younger than 5 years of age. Most studies focused on adoles-
cents and teenagers.
The majority of studies suggested a shorter sleep duration
was associated with either an increased risk of hypertension or
actual hypertension. However, the denition of “short/shorter”
sleep was different between the studies. For children > 5
years, studies suggested a shorter sleep duration (< 10 hours,
18
some < 9 hours,
19
some < 8 hours,
20,21
and one < 5 hours
22
) was
associated with either an increased risk of hypertension or ac-
tual hypertension. One study showed an increased odds ratio
of hypertension in girls who slept > 9.5 hours.
23
Another study
suggested that < 10 hours of sleep was associated with hypoten-
sion (systolic blood pressure < 100 mm Hg) in preschoolers.
18
1553
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
Conversely, there were also data to suggest no adverse effect of
sleep characteristics on cardiovascular health.
24–26
In summary, evidence indicates that shorter sleep duration
of < 5 hours is associated with increased risk of hypertension.
However, there is some suggestion that in girls regularly sleep-
ing more than 9.5 hours, hypertension risk is increased.
3.3 Metabolic Health
Many studies in the metabolic domain specically targeted the
relationship between sleep duration and overweight/obesity.
Other metabolic parameters studied included: waist circum-
ference, insulin resistance (HOMA-IR), bone mineral content,
triglycerides, C-reactive protein, HbA1c, leptin, and ghrelin.
Most were cross-sectional studies of community-based popu-
lations. The number of participants in studies ranged from 62
to 81,390.
Most studies demonstrated a negative association between
sleep duration and overweight/obesity. Shorter sleep dura-
tions were also associated with increased risk for developing
overweight/obesity. Two meta-analyses found sleep duration
inversely correlates with obesity in children 0–18 years.
27,28
For each hour increase in sleep, the risk of overweight/obesity
decreased. Children under age 10 years show a more linear
dose-response relationship of sleep duration and weight status.
Additionally, there is evidence of a stronger inverse relation-
ship for sleep duration and weight status in boys compared
with girls.
28
A longitudinal study of 915 children aged 6 months to 3
years, showed infant sleep duration of less than 12 hours per
day was associated with higher body mass index (BMI) z
scores and increased odds of overweight during subsequent
preschool years.
29
Similarly, in a cohort study of 1,930 children
ages 0–13 years, in younger children, ages 0–4 years, sleep du-
ration of less than 11 hours was subsequently associated with
increased risk of being overweight/obese. However for chil-
dren ages 5–13 years, sleep duration was not associated with
subsequent weight status.
30
Other cohort studies report similar
ndings.
31
A large cross-sectional study of 3,875 infants and
3,844 children (up to age 7 years) showed that sleep duration
did not predict obesity; however, obese children ages 6 to 7
years were found to sleep approximately 30 minutes less than
non-obese children.
32
In a cross-sectional study of 1,229 chil-
dren ages 5 to 11 years, children who slept less than 10 hours
per weeknight were 5 times more likely to be overweight than
those who slept at least 12 hours on weeknights.
33
In another
large cross-sectional study of 8,274 children ages 6 to 7 years
old, children with sleep duration shorter than 10 hours had an
increased odds ratio to develop obesity.
34
In a cross-sectional
study of 6,576 children, ages 7–11 years, children who slept < 9
hours per night had a higher risk for overweight, obesity, and
abdominal obesity compared to children who slept 10–11
hours.
35
In a study of 319 children ages 10–17 years, total sleep
time was negatively correlated with overweight/obese status.
36
Similar ndings were observed in a larger cross-sectional study
of 6,324 children ages 7–15 years. Boys who slept < 10 hours
per night had increased odds of overweight compared to chil-
dren sleeping > 10 hours.
37
In 3,311 children 12.5 to 17.5 years,
shorter sleep duration < 8 hours was associated with increased
BMI, body fat, and waist and hip circumferences.
38
A cohort
study of 1,303 children aged 5–29 months showed that chil-
dren sleeping < 10 hours per night consumed approximately
50 more kcal per day than children sleeping 11–12 hours,
39
sug-
gesting that changes in appetite may be a possible mechanism
for a relationship between short sleep and weight status. Of
note, one study of children ages 6–17 years reported no inde-
pendent association between insufcient sleep and childhood
obesity; however, no sleep duration information was provided
by parents.
40
In terms of other metabolic parameters, in a cohort of
652 children, chronic short sleep duration was associated
with higher waist circumference, higher insulin levels, and
greater HOMA-IR attributed to adiposity.
41
Higher HOMA
Indices were also observed in high school-aged children who
slept < 6.48 hours.
42
In children ages 4–7 years, there was in-
creased bone mineral content in children who slept longer than
8 hours.
43
A sample of 62 obese 8- to 17-year-old children studied
with polysomnography (PSG) showed a U-shape curve for
metabolic parameters such as HbA1c and insulin suggesting
an ideal range of 7.5–8.5 hours of sleep for this group of chil-
dren.
44
A U-shape curve was also observed in a study of 387
children ages 13–17 years, where HOMA-IR was 20% higher
when sleep duration was < 5 hours or > 10.5 hours.
45
Furthermore, higher C-reactive protein was observed in
13–17 year old children with < 9 hours sleep duration.
46
In summary, short sleep duration is associated with an in-
creased risk for overweight/obesity, particularly in younger
children < 10 years, and in boys. There is also evidence that
short or long sleep duration is associated with disruption of
other metabolic parameters including appetite and glucose/in-
sulin metabolism.
3.4 Mental Health
The variables of interest in the mental health domain related
to mood (e.g., depression, anxiety, suicidality, emotional regu-
lation, irritability and self-esteem); risk-taking behaviors (e.g.,
drug use); problematic behaviors (e.g., deance and tantrums);
and attention-decit/hyperactivity disorder (ADHD) symp-
toms (e.g., hyperactivity, impulsivity, and inattentiveness).
Studies included approximately 100 to 30,000 participants.
Limited data were available for children in the 4 months to
less than 12 months age range. One study looked at the longitu-
dinal sleep trajectories of approximately 3,000 children begin-
ning at age 0–1 year with follow-up at age 6–7 years.
9
Those
children who were persistent short sleepers and poor sleepers
had more difculties with emotional, social and physical func-
tioning at age 6–7 years when compared to “typical sleepers”
who slept approximately 14.5 hours of sleep at age 0–1 year
and 10.75 hours of sleep at age 6–7 years. Similarly, there were
few studies on sleep duration and emotional/mental health
within the 12 month to < 3 year old and 3 to < 6 year old age
categories. One study collected almost 33,000 parental sur-
veys regarding child sleep duration and the emotional and be-
havioral regulation of these children at 18 months and 5 years
of age.
47
Children who had short sleep duration of ≤ 10 hours
at 18 months were at signicantly greater risk of concurrent
1554
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
and subsequent incident emotional and behavioral problems
compared to a reference group of children receiving at least 13
hours of sleep at 18 months.
47
Studies reviewed for children ages 6–13 years of age fo-
cused on associations between total sleep duration and affect,
emotional regulation, irritability, relationships with peers/
family, and perceived health. Experimental studies of sleep re-
striction or sleep extension showed that participants sleeping
more than 9 hours (mean 9.8 hours) had better emotional labil-
ity scores and less restless/impulsive behaviors per teacher re-
ports compared to those sleeping an average of 8.4 hours.
48
In
a similar study, children with a mean of 9.3 hours of sleep had
signicantly higher positive affect scores and parent-reported
emotional regulation compared to children sleeping a mean of
8.1 hours.
49
In contrast, no group differences were detected in
negative affective scores and child-reported emotional regula-
tion ratings. In cross-sectional studies, data were more mixed.
For instance, impulsivity scores were signicantly higher
among children ages 7–8 years sleeping < 7.7 hours compared
to those sleeping > 7.7 hours, but no group differences were
found in total ADHD global scores.
50
Likewise, there were no
relationships between children sleeping less than 10 hours and
their affective scores or reported peer/family relationships, but
those sleeping ≥ 10 hours reported better overall health.
15
In contrast, the literature review showed a clearer relation-
ship between sleep duration and mental health among adoles-
cents, 13–18 years of age. Adolescents sleeping ≥ 9 hours of
sleep had signicantly better life satisfaction scores, fewer
general health complaints, and better quality relationships
with family compared to those sleeping less.
15
Of greatest con-
cern in the adolescent population are associations between
short sleep duration and suicidal thoughts/behaviors and sub-
stance abuse. In one cross-sectional survey of 27,939 adoles-
cents, participants who slept 7–8 hours reported less feelings
of hopelessness, less tobacco use, less alcohol use, less illicit
drug use, fewer suicidal thoughts, and fewer suicidal attempts
compared to participants who reported sleeping 6–7 hours per
night.
51
Of note, this study showed a negative correlation be-
tween more sleep and less concerning behaviors, but after 9
hours of sleep, an increase in these behaviors was noted. This
nding suggests a U-shape curve to sleep among adolescents
in which too little or too much sleep is associated with mental
health problems and substance abuse. To this point, another
study showed that teens sleeping ≤ 5 hours and ≥ 10 hours had
more suicidal attempts than those sleeping 8 hours per night.
52
In summary, there are limited data for infants 4 months to 1
year, but based on the literature, 14.5 hours of sleep seems ap-
propriate. Available longitudinal data on sleep duration for tod-
dlers suggests that at least 13 hours of sleep are benecial for
future mental health outcomes. In school-aged children, there
are conicting data, but children sleeping at least 10 hours re-
port less health complaints and children with < 8 hours of sleep
have increased reports of ADHD behaviors. Experimental data
suggest at least 9 hours of sleep is necessary for adequate be-
havioral functioning. In teens, data suggests that 8–9 hours of
sleep seems optimal for mental health and < 8 hours is associ-
ated with increased inappropriate behavior, including suicidal
attempts, and substance abuse. In this population, more than
10 hours of sleep was also associated with an increase in sui-
cidality, although causality cannot be ascertained.
3.5 Immunologic Health
The panel reviewed only 13 studies with respect to loosely
dened immunological health and sleep duration. All stud-
ies were cross-sectional, observational, or cohort design, and
none were randomized controlled studies. The number of par-
ticipants varied from as few as 54 to just under 1,500. The ma-
jority of study participants were older children, adolescents,
and teenagers. Sleep duration was measured via a mix of self-
report, parent report, actigraphy, or in some cases, the method
of measurement was not even reported.
One study suggested that sleep duration of 8–8.9 hours was
associated with a healthier immune prole (cortisol, immune
cell counts, and cytokines).
53
Another study noted an inverse
relationship between CRP and sleep duration with higher
CRPs noted in those sleeping less than 8 hours.
46
Other studies
showed no relationship between sleep variables and inamma-
tion (brinogen, IL-6, and CRP).
54
No studies suggested too
much sleep was harmful.
In summary, based on very limited and less than ideal qual-
ity evidence, it would seem that sleep durations less than 8
hours are associated with worse overall immunological health,
and that optimal sleep is between 8–9 hours for older children
and adolescents.
3.6 Human Performance
The human performance domain included a wide range of out-
comes including: neuropsychological testing (e.g., emotional
responses, cognitive performance, academic achievement);
school grades; rating scales for attention, behavior or execu-
tive functioning; ratings scales for behavioral persistence (sus-
tained attention), well-being, health behaviors and complaints;
suicide or accident risk; subjective reports of daytime sleepi-
ness; and measured electroencephalography (EEG) arous-
als. Most studies were cohort or cross-sectional studies of
community-based populations; prospective, longitudinal co-
hort data were rare. Some studies utilized a case-control study
design. Other studies used an experimental design to compare
the effects of sleep deprivation or sleep extension to the control
condition. The number of participants ranged from less than
100 in most of the case-control or experimental studies to over
3,000 in some of the cohort studies.
In a small experimental sample of 10 children aged 30–36
months, loss of a daytime nap resulting in total 24-h sleep du-
ration of less than 11 hours was associated with more nega-
tive emotional responses.
55
In preschoolers, sleep durations
of less than 8 hours in the previous 24 hours were associated
with a more than 2-fold increased risk of accidental falls.
56
In
a large prospective longitudinal cohort study of 1,492 children
aged 6 years, it was found that children with sleep durations
less than 10 hours as toddlers and preschoolers had higher
parent-reported hyperactivity indices and lower cognitive per-
formance.
57
In 812 school-aged children, sleeping less than 9
hours per night was associated with worse teacher-reported ac-
ademic achievement, but did not impact domains of attention,
motivation, or relationships.
58
In 74 children ages 6–12 years,
1555
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
one week of sleep restriction to 6.5 hours resulted in increases
in teacher-reported academic difculties and attentional prob-
lems compared with “optimized” sleep (at least 9 hours).
59
In
33 children ages 7–11 years with a mean baseline sleep dura-
tion of 9 hours 20 minutes, sleep extension of approximately
30 minutes was associated with improved alertness; whereas
modest sleep restriction (approximately 1 hour) had opposite
effects.
48
Among 77 children ages 9–12 years with a baseline
sleep duration of 8.1 hours, cognitive performance testing im-
proved with a 1-hour extension, but worsened with a 1-hour re-
striction.
60
In 32 children ages 8–12 years with a baseline sleep
duration of 8.8 hours, 4 days of sleep restriction to 8 hours
compared to 4 days of sleep extension to 9.3 hours, resulted in
impairment of memory and attention.
49
Several studies reported on both school-age and teen par-
ticipants. Self-reported sleep durations of less than 10 hours
for children and less than 9 hours for adolescents were asso-
ciated with increased somatic health complaints (higher odds
ratios) when compared to their full sleep conditions.
15
Among
3,011 children 6 to 16 years, short sleep duration (less than
the median hours for each of 4 age groups dened by school
grade levels) was associated with self-reported daytime tired-
ness in school.
61
In a large sample of 1,691 participants ages
10–19 years, sleep duration that was one hour less than “op-
timum” self-reported sleep (which varied by age) predicted
lower academic achievement scores, with a larger effect on
the older group.
62
This study also suggested a U-shape effect
where much longer sleep durations were associated with worse
performance.
62
In a small sample of 16 adolescents, 5 nights of
experimental sleep restriction to 6.5 hours resulted in inatten-
tion, diminished learning and lowered arousal in a simulated
classroom when compared to a “healthy” sleep condition of 8
hours.
63
Lower parent-ratings of executive function and par-
ticipant performance were associated with self-reported sleepi-
ness in an urban cohort of 236 teens, but not with sleep duration
measured by actigraphy.
64
Among a large cohort of 2,716 teens,
sleeping less than 8 hours per night was related to more self-
reported tiredness, inferior behavioral persistence (sustained
attention), less positive attitude toward life, and lower school
grades, as compared to sleeping longer durations.
65
Daytime
tiredness and behavioral persistence mediated the relationship
between short sleep duration and positive attitude toward life
and school grades. Except for self-reported tiredness, there
were no differences between sleeping 8–9 hours and sleeping
more than 9 hours. Students who started school 20 minutes
later received reliably more sleep and reported less tiredness.
65
In a large cohort of 1,564 teens, sleeping less than 8 hours was
associated with lower cognitive performance for boys, but not
girls.
66
Finally, in a large cohort of 1,362 teens, sleeping less
than 8 hours, compared to more than 9 hours, per night was
associated with greater risk of suicide, while sleeping 8 to 9
hours was not.
67
In summary, among various outcomes that comprise human
performance, there are sufcient and compelling data to sup-
port recommendations for sleep durations of at least 11 hours
for toddlers, 10 hours for preschoolers, 9 hours for school-
aged children, and 8 hours for teenagers to support optimal
performance.
3.7 Developmental Health
Many studies in the developmental health domain targeted
the associations between sleep duration and neurobehavioral
and neurocognitive measures. There was signicant overlap in
studies reviewed for this domain, most often with the mental
health and human performance domains. Sample sizes ranged
from 10 participants (randomized cross-over design) to 35,956
(meta-analysis). There were often methodological issues about
assumptions of directionality of relationships and variation
in reference categories used for “normal sleep duration.” The
covariates differed widely by study and there was signicant
heterogeneity in outcomes. Results also differed by gender and
ethnicity. The panel members noted that besides being associ-
ated with child development, short sleep duration has the po-
tential to affect parent-child interactions, which increases the
complexity of health interactions.
Short sleep duration has a negative association with cog-
nitive performance in a number of age groups based on
longitudinal (< 10 hours,
57
< 9 hours,
58
< 11 hours
68
) and cross-
sectional (< 9 hours
15,69
), (< 8 hours
70
), (< 11 hours
71
) studies;
however, some studies have reported a U-shape relationship
with too much sleep time associated with poorer cognitive
performance.
68
For children aged 11–13 months, the proportion of total
daily sleep occurring at night has been positively correlated
with the development of communication and problem solv-
ing skills.
72
Young children’s poorer language function was
positively associated with shorter sleep hours during the
night.
73
For preschoolers (4 years) and school-aged children
(10 years), short sleep duration (< 11 hours) was negatively
associated with receptive vocabulary.
74
Poor emotional regu-
lation and reactivity have been associated with short sleep
duration (30–36 month-olds,
55
18-month-olds
47
for < 13 hours,
and 2.5–6 year-olds for < 10 hours
57
), but one study reported
a U-shape relationship.
75
Shorter sleep duration has been as-
sociated with poorer morning and daytime mood in infants.
76
As mentioned above in the mental health domain, short sleep
duration at 18 months (< 13 hours) predicted more emotion-
ally reactive and aggressive behavior at 5 years.
47
Persistent
short sleep duration (from 0 to 7 years) has been associated
with higher levels of child irritability and poorer emotional
functioning.
9
Additionally, naps may be important. Missing one nap by
preschoolers produced more negative emotional responses
55
and nap provision improved toddlers’ performances on a gen-
eralization task
77
and grammatical language patterns 24 hours
later
78
compared with non-nap groups.
In one study, sleeping less than 8 hours per night was associ-
ated with poorer cognitive performance on reasoning abilities
for adolescent boys but not adolescent girls.
66
Another study
showed that adolescents had positive associations between
sleeping less than 8 hours and poorer school grades.
65
The
single meta-analysis of 35,956 children aged 5 to 12 years did
not specify sleep duration, but reported that longer sleep du-
ration was associated with better cognitive performance (e.g.,
implicit memory, intelligence, and school performance) and
fewer behavioral problems.
79
Shorter sleep duration has been
linked to school-aged children’s and adolescents’ attention

1556
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
problems,
49,59,63,80
restless/impulsive behavior
48
(< 9 hours) and
deterioration in vigilance
60
(30-minute sleep restriction).
The cited range for normal sleep duration is wide, ranging
from 14.5 hours during infancy
9
to 9–10 hours at school entry
and pre-adolescent children
9,81,82
to about 8.5 hours in late ado-
lescence.
83
Studies do not consistently exclude forms of sleep
problems. For example, in younger children, the proportion of
sleep at night, sleep efciency and difculty settling demon-
strate the complexity of explicating relationships between sleep
duration and developmental well-being.
72,73
A large, cross-sec-
tional study of 4–9-year-olds did not demonstrate consistent
relationships between sleep duration thresholds and learning,
based on parent-completed 24-hour time-use diaries.
84
Only at
ages 6 to 7 years did they report a positive relationship be-
tween at least 10 hours of sleep per night and mathematical
thinking, language, and literacy based on cutoff points on di-
agnostic categories from teacher report. The ndings were dif-
cult to interpret because plots showed most children averaged
between 10 to 12 hours of sleep per night. Thus the variance
in sleep duration appeared quite limited and the dichotomizing
of measures into problem/no problem reduced the information
available for testing.
In summary, there appears to be consistent relationships be-
tween inadequate sleep duration and development of children’s
cognition, language, memory, executive function, emotional
regulation, and reactivity.
3.8 Longevity
This area focused on sleep patterns in pediatric age groups
and how those patterns affect longevity. Seventy-four studies
were identied in the initial review. Thirty-seven of the stud-
ies associated sleep duration with accidents, suicidal ideation,
insomnia, stress, depression, or anxiety. The other 37 studies
associated sleep duration with cardiovascular, metabolic, pul-
monary, allergy/atopy, and obesity-related conditions. None
of the articles either evaluated or demonstrated any direct re-
lationship between sleep duration and longevity in the pedi-
atric population. Although some of the associations, such as
increased risk of suicidal ideation or adverse cardiovascular
risk factors could impact longevity, those outcomes were not
specically addressed in any of the studies. Therefore, no rec-
ommendation was made for optimal sleep duration at any age
as related to longevity.
4.0 STRENGTHS AND WEAKNESSES OF THE
LITERATURE
The panel recommendations were based on literature charac-
terized by several strengths. Taken together, studies on sleep
duration include data on hundreds of thousands of children
and teenagers, studied across several continents, aggregated
over several decades. The studies include cross-sectional and
longitudinal epidemiologic designs, randomized controlled tri-
als, meta-analyses, and a range of other designs. Studies in the
mental health category appear to have the strongest evidence.
A number of important limitations in both epidemiologic
and lab-based studies are also evident. First, most of the
studies reviewed were cross-sectional, thus ndings were cor-
relational, precluding statements of causation. Second, sleep
duration was ascertained for a limited time frame around the
assessment, with multiple ages grouped together despite ob-
vious differences in development. For example, some studies
included participants aged 8–18 years, and it is unknown how
the results would have differed had the participants’ data been
grouped as pre-adolescent vs adolescent with a different age
cut-off. Some studies may have had insufcient adjustment
for confounders. Additionally, without prospective, long-term
studies, pediatric sleep duration data on outcomes such as lon-
gevity are lacking.
Furthermore, the methods of sleep assessment present limi-
tations. Most studies described sleep duration obtained from
parental report, or child report when age-appropriate. This
may be less accurate than averages from daily report on sleep
diaries. Parent- or self-reported duration may over- or under-
estimate sleep duration measured objectively by actigraphy or
polysomnography. Additionally, studies varied in how sleep
duration was reported, i.e., per 24 hours or overnight sleep. Du-
ration reporting was discussed extensively by panel members
to determine the best means to evaluate the available literature
and provide appropriate sleep duration recommendations in the
predened age groups of children. Survey questions often had
good face validity, but most were not formally validated with
psychometric analyses. Multiple surveys also gathered health
outcomes such as height, weight, and lists of medical problems,
by parental or child report; relying on these reports may be a
source of measurement error. Also, measures of sleep duration
often do not capture information about the regularity of sleep
patterns, the timing of sleep, or the quality of sleep, all of which
could directly affect sleep duration and health outcomes.
Experimental designs have important limitations as well.
Most studies included short periods of sleep duration manip-
ulation, almost always < 2 weeks. The acute effects of sleep
deprivation may not approximate real-world effects of chronic
sleep deprivation. Few studies examined sleep duration in the
range between 8 and 12 hours. This likely reects the aim of
experimental studies, which often try to maximize differences
in outcomes by contrasting extreme sleep duration groups. The
absence of experimental groups in these sleep duration ranges
creates some uncertainty in recommendations due to lack of
data. Many studies also lack generalizability because of small
sample sizes that may not represent the population in terms
of age, sex, race, ethnicity, socioeconomic status, or health
history. Many studies investigated groups of children across
multiple ages at different developmental stages, but reported a
single result. PSG measurements of sleep duration may not be
an accurate measure of typical sleep duration given the differ-
ent sleep environment (lab) and weak correlations with paren-
tal or child self-reported duration.
5.0 VOTING SUMMARY
Voting results from all 3 rounds are presented in Figures 1–3.
Napping was discussed for age appropriate groups, and re-
ected in the nal recommendations for children through age

1557
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
5 years explicitly, with the understanding that some healthy
children up to age 7 years may habitually nap. The panel dis-
cussed several reasons for why short or long sleep durations
may be inappropriate for each age group after incorporating
ndings from the literature and criteria for sleep disorders. All
values are per 24 hours.
For infants, there was consensus that < 12 hours of sleep
per 24 hours was inappropriate to support optimal health.
There was also consensus that a range of 12 to 16 hours was
appropriate to support optimal infant health. Consensus could
not be reached on 16 to 18 hours due to uncertainty given the
lack of data in this sleep duration range. However, there was
consensus that ≥ 18 hours of sleep was inappropriate. There
was also consensus that no recommendations could be made
in infants < 4 months of age, due to the paucity of published
outcomes in infants this young.
For children aged 1 to < 3 years, there was consensus that
sleep duration of < 10 hours was inappropriate. There was con-
sensus that 11 to 14 hours per 24 hours was appropriate. Un-
certainty was observed in the 10–11 hour range and 14 to 16
hour range, with panel consensus that sleep times longer than
16 hours in this age group were inappropriate.
For children aged 3 to < 6 years, there was consensus
that sleep duration of < 10 hours or more than 14 hours was
inappropriate. There was consensus that 10–13 hours of sleep
was appropriate. Uncertainty existed in the 13 to 14 hour dura-
tion range. The panel discussed that the sleep needs of a 3-year
old preschooler may be vastly different than the sleep needs of
a 6-year old rst-grader.
For children aged 6 years to < 13 years, there was consen-
sus that sleep duration of 9 to 12 hours was appropriate and
that > 13 hours was inappropriate. There was uncertainty if
12–13 hours of sleep duration was appropriate.
For teenagers aged 13 to 18 years of age, there was consen-
sus that < 8 hours or > 10 hours of sleep on a regular basis was
inappropriate. There was consensus that 8 to 10 hours was ap-
propriate for optimal health.
The panel discussed the merits of recommending sleep du-
rations for multiple age groups vs collapsing all age groups
to recommend 1 single sleep duration threshold. Implicit to a
range recommendation is the conclusion that sleep duration
above a certain amount of sleep is detrimental to health. The
literature supported a clear cut-off in optimal sleep duration in
the teenager group, as there were unambiguously better health
outcomes within the recommended range, and clear negative
outcomes and an increased likelihood of sleep disorders when
nightly sleep durations were < 8 hours or > 10 hours. Within
other age groups, due to the wide age ranges in studies and lack
Figure 2—Round 2 voting results.
Round 2 voting was based on voting across all age groups under the following seven domains: cardiovascular health, developmental health, human
performance, general health, immunology, mental health and metabolic health.

1558
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
of published literature, there was often uncertainty on the outer
ends of the agreed upon appropriate sleep duration ranges. The
panel also discussed consideration of nap duration for age ap-
propriate children. With these considerations in mind, the
panel voted to recommend ranges for each age group. No age
groups were collapsed and no age groups were further sepa-
rated during the in-person meeting because voting in Round 1
had already taken place.
6.0 DISCUSSION
Sleep is a necessity for health. Meeting the need for sleep dura-
tion, timing, regularity, and quality requires volitional behav-
iors by parents and children, which are partially dictated by
genetic and physiologic factors. However, a large proportion
of inter-individual variability in sleep is likely explained by
psychological, behavioral, social, cultural, and environmental
factors. Sleep disorders also contribute to this variability.
For reasons stated above, the panel focused solely on the
dimension of sleep duration, while recognizing the importance
of other factors such as timing, regularity, and quality. The rec-
ommendations provide sleep durations that promote optimal
pediatric health, but do not address other sleep factors. The
panel excluded studies that focused on sleep factors other than
sleep duration and studies that focused on total sleep depri-
vation (no sleep for 24 hours). Total sleep deprivation is not
sustainable and thus not reective of habitual sleep, which was
the focus of the panel. In general, the total sleep time is high
in infants and toddlers, with gradual reduction over time as
one approaches pre-adolescence and adolescence. This change
parallels the ontogeny of cerebral metabolism that was studied
in 100 healthy children using positron emission tomography.
85
The reduction in total sleep time over the rst decade is felt to
be related to an initial overproduction, and subsequent pruning
away of unnecessary synapses.
85
All panel members agreed that too little sleep for each age
group was unhealthy. The panel discussed thoroughly the ap-
propriateness of longer sleep durations for each age group. The
panel discussed the higher likelihood of sleep disorders often
being associated with longer sleep times, which was then in-
congruent with sleep duration for optimal health. Another con-
sideration was the lack of studies in children on sleep extension.
There were a few U-shape curves that showed that both, too
little and too much sleep were associated with poorer outcomes.
The panel strongly encourages future experimental studies to
examine the effects of sleep extension on health outcomes.
The panel recommendations reect typical or habitual sleep
duration, i.e., the ideal average sleep duration. However, the
panel discussed that sleep duration in the real world is a dy-
namic process. Many children, particularly those who have ex-
perienced a delay in their circadian rhythms in puberty, have
variable sleep schedules depending on school start times, work,
and extracurricular activities that may curtail sleep on week-
days and extend sleep on weekends. More studies are needed
to better characterize effects of this “social jet lag.”
Figure 3—Round 3 voting results.
Round 3 voting is based on voting summary across all age groups.

1559
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
The panel discussed heterogeneity of sleep duration
measurement at length: subjective report vs (more) objective
actigraphy, parental report vs child self-report, time in bed vs
time asleep, and inclusion vs exclusion of naps. Several stud-
ies have shown that self-report may differ substantially from
objective measurement.
Polysomnography and actigraphy were utilized in some
studies as objective measurements of sleep duration, and the
panel discussed the strengths and limitations of these studies.
Actigraphy may over-estimate sleep duration relative to self-
report in poor sleepers. PSG directly records sleep, however,
other factors such as “rst night effect” or logistics such as
set wake up times to end PSG recordings may be in place and
thus not accurately reect a typical night of sleep. Home sleep
apnea testing is not currently recommended in children, and
also does not provide accurate reection of sleep time. As
technology improves and the use of activity trackers becomes
more widespread in the pediatric population, more data will be
available to better measure sleep duration and compare time
and effects within large participant samples.
7.0 FUTURE DIRECTIONS
The recommendations of the panel are intended to be a rst
step towards promoting adequate sleep duration for all chil-
dren. The panel reviewed existing literature to achieve con-
sensus, and realized that serious gaps in knowledge exist in
the pediatric population. As more high-quality literature be-
comes available, the recommendations may change in the fu-
ture. Based on this process, specic areas for future research
consideration are presented:
1. Implement improved sleep duration measures and
study designs, including intervention studies. As
child development changes signicantly from year
to year, it is imperative to study narrower age groups,
with validated studies and intervention designs to
better delineate sleep deprivation effects on important
outcomes such as mental health, physical health, and
cognitive functioning. Small preliminary studies
have begun to explore the effects of sleep extension
on health and functioning in children. More studies
are recommended (i.e., between 8 and 10 hours in
adolescents) to systematically vary sleep opportunity
in discrete steps between the upper and lower amounts
using objective measurements of sleep physiology
and cognitive performance. These studies should also
examine longer time periods (e.g., 30 days), including
weekdays and weekend days, to develop more precise
dose-response curves for sleep and recovery effects
within the ranges most often reported by children and
parents. Studies that mimic typical sleep-wake cycles
and lifestyles in each age group are needed.
2. Investigate downstream mechanisms linking habitual
sleep duration to health and functioning. Intervention
studies are needed to help clarify whether modifying
sleep duration improves health outcomes in children.
Such studies will help to explain whether sleep
duration has a causal role in health and functioning vs
operating as a marker of other processes.
3. Delineate the upstream physiologic, behavioral, social,
and environmental factors that may play a role in sleep
duration and health outcomes. Studies are needed to
identify how genetics relate to individual sleep need
and the response and resilience to sleep loss. Studies
are also needed that explore the roles of race, ethnicity,
socioeconomic factors, neighborhoods, school start
times, and other factors that contribute to sleep
duration.
4. Identify biomarkers of sleep need or sleep deprivation.
Inexpensive, reliable, and feasible biomarkers could
advance the goals of clinical care, public health, and
public policy. In the future, biomarkers may allow
clinicians to provide more accurate sleep schedule
recommendations to children, parents, and policy
makers to facilitate policy decisions (e.g., school start
times and teen driving). Biomarkers may greatly assist
research assessment of the long term consequences of
sleep deprivation.
CONCLUSIONS
The 13-member panel used a modied RAND Appropriate-
ness Method to generate consensus recommendations for the
amount of sleep to promote optimal health in children. Mul-
tiple rounds of evidence review, discussion and voting were
conducted to arrive at the nal recommendations. Additional
research on the role of sleep duration at different stages in a
child’s growth and development will help increase the aware-
ness of the importance of sleep and lead to improved health
and well-being for children and families.
REFERENCES
1. de Bruin EJ, van Run C, Staaks J, Meijer AM. Effects of sleep manipulation
on cognitive functioning of adolescents: a systematic review. Sleep Med Rev
2016: in press.
2. Vriend J, Davidson F, Rusak B, Corkum P. emotional and cognitive impact of
sleep restriction in children. Sleep Med Clin 2015;10:107–15.
3. Cassoff J, Bhatti JA, Gruber R. The effect of sleep restriction on
neurobehavioural functioning in normally developing children and adolescents:
insights from the attention, behaviour and sleep laboratory. Pathol Biol (Paris)
2014;62:319–31.
4. Fitch K, Bernstein S, Aguilar M, et al. The RAND/UCLA Appropriateness
Method User’s Manual. Santa Monica, CA: RAND, 2001.
5. Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended amount of sleep
for pediatric populations: a consensus statement of the American Academy of
Sleep Medicine. J Clin Sleep Med 2016;12:785–6.
6. US Department of Health and Human Services, Sleep Health Objectives.
Accessed February 25th, 2016. Available from: https://www.healthypeople.
gov/2020/topics-objectives/topic/sleep-health/objectives.
7. Oxford Center for Evidence Based Medicine. Accessed March 15, 2016.
Available from: http://www.cebm.net/ocebm-levels-of-evidence/.
8. Scott N, Blair PS, Emond AM, et al. Sleep patterns in children with ADHD:
a population-based cohort study from birth to 11 years. J Sleep Res
2013;22:121–8.
1560
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
9. Magee CA, Gordon R, Caputi P. Distinct developmental trends in sleep
duration during early childhood. Pediatrics 2014;133:e1561–7.
10. Valent F, Brusaferro S, Barbone F. A case-crossover study of sleep and
childhood injury. Pediatrics 2001;107:E23.
11. Wang H, Sekine M, Chen X, Yamagami T, Kagamimori S. Lifestyle at
3 years of age and quality of life (QOL) in rst-year junior high school
students in Japan: results of the Toyama Birth Cohort Study. Qual Life Res
2008;17:257– 65.
12. Quan SF, Goodwin JL, Babar SI, et al. Sleep architecture in normal Caucasian
and Hispanic children aged 6-11 years recorded during unattended home
polysomnography: experience from the Tucson Children’s Assessment of
Sleep Apnea Study (TuCASA). Sleep Med 2003;4:13–9.
13. Williams RL, Karacan I, Hursch CJ. Electroencephalography (EEG) of human
sleep: clinical applications. New York: John Wiley & Sons, 1974.
14. Olds T, Blunden S, Petkov J, Forchino F. The relationships between sex, age,
geography and time in bed in adolescents: a meta-analysis of data from 23
countries. Sleep Med Rev 2010;14:371–8.
15. Segura-Jimenez V, Carbonell-Baeza A, Keating XD, Ruiz JR, Castro-Pinero
J. Association of sleep patterns with psychological positive health and health
complaints in children and adolescents. Qual Life Res 2015;24:885–95.
16. Lam LT, Yang L. Short duration of sleep and unintentional injuries among
adolescents in China. Am J Epidemiol 2007;166:1053–8.
17. Milewski MD, Skaggs DL, Bishop GA, et al. Chronic lack of sleep is associated
with increased sports injuries in adolescent athletes. J Pediatr Orthop
2014;34:129–33.
18. Sampei M, Murata K, Dakeishi M, Wood DC. Cardiac autonomic hypofunction
in preschool children with short nocturnal sleep. Tohoku J Exp Med
2006;208:235–42.
19. Guo X, Zheng L, Li Y, et al. Association between sleep duration and
hypertension among Chinese children and adolescents. Clin Cardiol
2011;34:774–81.
20. Azadbakht L, Kelishadi R, Saraf-Bank S, et al. The association of sleep
duration and cardiometabolic risk factors in a national sample of children and
adolescents: the CASPIAN III Study. Nutrition 2013;29:1133–41.
21. Kuciene R, Dulskiene V. Associations of short sleep duration with
prehypertension and hypertension among Lithuanian children and
adolescents: a cross-sectional study. BMC Public Health 2014;14:255.
22. Lee JA. Park HS. Relation between sleep duration, overweight, and metabolic
syndrome in Korean adolescents. Nutr Metab Cardiovasc Dis 2014;24:65–71.
23. Paciencia I, Barros H, Araújo J, Ramos E. Association between sleep duration
and blood pressure in adolescents. Hypertens Res 2013;36:747–52.
24. Berentzen NE, Smit HA, Bekkers MB, et al. Time in bed, sleep quality
and associations with cardiometabolic markers in children: the Prevention
and Incidence of Asthma and Mite Allergy birth cohort study. J Sleep Res
2014;23:3–12.
25. Rey-Lopez JP, de Carvalho HB, de Moraes AC, et al. Sleep time and
cardiovascular risk factors in adolescents: the HELENA (Healthy Lifestyle in
Europe by Nutrition in Adolescence) study. Sleep Med 2014;15:104–10.
26. Sung V, Beebe DW, Vandyke R, et al. Does sleep duration predict metabolic
risk in obese adolescents attending tertiary services? A cross-sectional study.
Sleep 2011;34:891–8.
27. Fatima Y, Doi SA, Mamun AA. Longitudinal impact of sleep on overweight and
obesity in children and adolescents: a systematic review and bias-adjusted
meta-analysis. Obes Rev 2015;16:137–49.
28. Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood
obesity? A systematic review and meta-analysis. Obesity (Silver Spring)
2008;16:265–74.
29. Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP, Gillman MW. Short
sleep duration in infancy and risk of childhood overweight. Arch Pediatr
Adolesc Med 2008;162:305–11.
30. Bell JF, Zimmerman FJ. Shortened nighttime sleep duration in early life and
subsequent childhood obesity. Arch Pediatr Adolesc Med 2010;164:840–5.
31. Diethelm K, Bolzenius K, Cheng G, Remer T, Buyken AE. Longitudinal
associations between reported sleep duration in early childhood and the
development of body mass index, fat mass index and fat free mass index until
age 7. Int J Pediatr Obes 2011;6:e114–23.
32. Hiscock H, Scalzo K, Canterford L, Wake M. Sleep duration and body mass
index in 0-7-year olds. Arch Dis Child 2011;96:735–9.
33. Duncan JS, Schoeld G Duncan EK, Rush EC. Risk factors for excess body
fatness in New Zealand children. Asia Pac J Clin Nutr 2008;17:138–47.
34. Sekine M, Yamagami T, Handa K, et al. A dose-response relationship between
short sleeping hours and childhood obesity: results of the Toyama Birth Cohort
Study. Child Care Health Dev 2002;28:163–70.
35. Meng LP, Liu AL, Hu X, et al. Report on childhood obesity in China
(10): association of sleep duration with obesity. Biomed Environ Sci
2012;25:133–40.
36. Drescher AA, Goodwin JL, Silva GE, Quan SF. Caffeine and screen time in
adolescence: associations with short sleep and obesity. J Clin Sleep Med
2011;7:337– 42.
37. Eisenmann JC, Ekkekakis P, Holmes M. Sleep duration and overweight among
Australian children and adolescents. Acta Paediatr 2006;95:956–63.
38. Garaulet M, Ortega FB, Ruiz JR, et al. Short sleep duration is associated with
increased obesity markers in European adolescents: effect of physical activity
and dietary habits. The HELENA study. Int J Obes (Lond) 2011;35:1308–17.
39. Fisher A, McDonald L, van Jaarsveld CH, et al. Sleep and energy intake in
early childhood. Int J Obes (Lond) 2014;38:926–9.
40. Hassan F, Davis MM, Chervin RD. No independent association between
insufcient sleep and childhood obesity in the National Survey of Children’s
Health. J Clin Sleep Med 2011;7:153–7.
41. Cespedes EM, Rifas-Shiman SL, Redline S, Gillman MW, Peña MM, Taveras
EM. Longitudinal associations of sleep curtailment with metabolic risk in mid-
childhood. Obesity (Silver Spring) 2014;22:2586–92.
42. Matthews KA, Dahl RE, Owens JF, Lee L, Hall M. Sleep duration and insulin
resistance in healthy black and white adolescents. Sleep 2012;35:1353–8.
43. Casazza K, Hanks LJ, Fernandez JR. Shorter sleep may be a risk factor for
impaired bone mass accrual in childhood. J Clin Densitom 2011;14:453–7.
44. Koren D, Levitt Katz LE, Brar PC, Gallagher PR, Berkowitz RI, Brooks LJ.
Sleep architecture and glucose and insulin homeostasis in obese adolescents.
Diabetes Care 2011;34:2442–7.
45. Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Association of short
and long sleep durations with insulin sensitivity in adolescents. J Pediatr
2011;158:617–23.
46. Martinez-Gomez D, Eisenmann JC, Gomez-Martinez S, et al.; AFINOS
Study Group. Sleep duration and emerging cardiometabolic risk markers in
adolescents. The AFINOS study. Sleep Med 2011;12:997–1002.
47. Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen L, Ystrom E,
Hysing M. Later emotional and behavioral problems associated with sleep
problems in toddlers: a longitudinal study. JAMA Pediatr 2015;169:575–82.
48. Gruber R, Cassoff J, Frenette S, Wiebe S, Carrier J. Impact of sleep extension
and restriction on children’s emotional lability and impulsivity. Pediatrics
2012;130:e1155–61.
49. Vriend JL, Davidson FD, Corkum PV, Rusak B, Chambers CT, McLaughlin
EN. Manipulating sleep duration alters emotional functioning and cognitive
performance in children. J Pediatr Psychol 2013;38:1058–69.
50. Paavonen EJ, Raikkonen K, Lahti J, et al. Short sleep duration and behavioral
symptoms of attention-decit/hyperactivity disorder in healthy 7- to 8-year-old
children. Pediatrics 2009;123:e857–64.
51. Winsler A, Deutsch A, Vorona RD, Payne PA, Szklo-Coxe M. Sleepless
in Fairfax: the difference one more hour of sleep can make for teen
hopelessness, suicidal ideation, and substance use. J Youth Adolesc
2015;44:362–78.
52. Fitzgerald CT, Messias E, Buysse DJ. Teen sleep and suicidality: results
from the youth risk behavior surveys of 2007 and 2009. J Clin Sleep Med
2011;7:351–6.
53. Perez de Heredia, Garaulet M, Gómez-Martínez S, et al. Self-reported
sleep duration, white blood cell counts and cytokine proles in European
adolescents: the HELENA study. Sleep Med 2014;15:1251–8.
54. Countryman AJ, Saab PG, Llabre MM, Penedo FJ, McCalla JR, Schneiderman
N. Cardiometabolic risk in adolescents: associations with physical activity,
tness, and sleep. Ann Behav Med 2013;45:121–31.
55. Berger RH, Miller AL, Seifer R, Cares SR, LeBourgeois MK. Acute
sleep restriction effects on emotion responses in 30- to 36-month-old
children. J Sleep Res 2012;21:235–46.

1561
Journal of Clinical Sleep Medicine, Vol. 12, No. 11, 2016
S Paruthi, LJ Brooks, C D’Ambrosio et al. Special Article
56. Boto LR, Crispim JN, de Melo IS, et al. Sleep deprivation and accidental fall
risk in children. Sleep Med 2012;13:88–95.
57. Touchette E, Petit D, Seguin JR, Boivin M, Tremblay RE, Montplaisir JY.
Associations between sleep duration patterns and behavioral/cognitive
functioning at school entry. Sleep 2007;30:1213–9.
58. Li S, Arguelles L, Jiang F, et al. Sleep, school performance, and a school-
based intervention among school-aged children: a sleep series study in China.
PLoS One 2013;8:e67928.
59. Fallone G, Acebo C, Seifer R, Carskadon MA. Experimental restriction of
sleep opportunity in children: effects on teacher ratings. Sleep 2005;28:1561–7.
60. Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension
on school-age children: what a difference an hour makes. Child Dev
2003;74:444–55.
61. Garmy P, Nyberg P, Jakobsson U. Sleep and television and computer habits of
Swedish school-age children. J Sch Nurs 2012;28:469–76.
62. Eide E. Sleep and Student Achievement. Eastern Econ J 2012;38.
63. Beebe DW, Rose D, Amin R. Attention, learning, and arousal of experimentally
sleep-restricted adolescents in a simulated classroom. J Adolesc Health
2010;47:523–5.
64. Anderson B, Storfer-Isser A, Taylor HG, Rosen CL, Redline S. Associations
of executive function with sleepiness and sleep duration in adolescents.
Pediatrics 2009;123:e701–7.
65. Perkinson-Gloor N, Lemola S, Grob A. Sleep duration, positive attitude toward
life, and academic achievement: the role of daytime tiredness, behavioral
persistence, and school start times. J Adolesc 2013;36:311–8.
66. Ortega FB, Ruiz JR, Castillo R, et al. Sleep duration and cognitive
performance in adolescence. The AVENA study. Acta Paediatr 2010;99:454–6.
67. Liu X. Sleep and adolescent suicidal behavior. Sleep 2004;27:1351–8.
68. Kocevska D, Rijlaarsdam J, Ghassabian A, et al. Early childhood sleep
patterns and cognitive development at age 6 years: the Generation R
Study. J Pediatric Psychol 2016;1–9.
69. Ravid S, Afek I, Suraiya S, Shahar E, Pillar G. Kindergarten children’s failure
to qualify for rst grade could result from sleep disturbances. J Child Neurol
2009;24:816–22.
70. Stea TH, Knutsen T, Torstveit MK. Association between short time in bed,
health-risk behaviors and poor academic achievement among Norwegian
adolescents. Sleep Med 2014;15:666–71.
71. Tso W, Rao N, Jiang F, et al. Sleep duration and school readiness of Chinese
preschool children. J Pediatr 2016;169:266–71.
72. Gibson R, Elder A, Gander P. Actigraphic sleep and developmental progress
of one-year-old infants. Sleep Biol Rhythms 2012;10:77–83.
73. Iemura A, Iwasaki M, Yamakawa N, et al. Inuence of sleep-onset time on the
development of 18-month-old infants: Japan Children’s cohort study. Brain
Dev 2016;38:364–72.
74. Seegers V, Touchette E, Dionne G, et al. Short persistent sleep duration
is associated with poor receptive vocabulary performance in middle
childhood. J Sleep Res 2016;25:325–32.
75. Carvalho Bos S, Gomes A, Clemente V, et al. Sleep and behavioral/emotional
problems in children: a population-based study. Sleep Med 2009;10:66–74.
76. Mindell J, Lee C. Sleep, mood, and development in infants. Infant Behav Dev
2015;41:102–7.
77. Horváth K, Liu S, Plunkett K. A daytime nap facilitates generalization of word
meanings in young toddlers. Sleep 2016;39:203–7.
78. Hupbach A, Gomez RL, Bootzin RR, Nadel L. Nap-dependent learning in
infants. Dev Sci 2009;12:1007–12.
79. Astill RG, Van der Heijden KB, Van IJzendoorn MH, Van Someren EJW.
Sleep, cognition, and behavioral problems in school-age children: a century of
research meta-analyzed. Psychol Bull 2012;138:1109–38.
80. Lo JC, Ong JL, Leong RLF, Gooley JJ, Chee MWL. Cognitive performance,
sleepiness, and mood in partially sleep deprived adolescents: the need for
sleep study. Sleep 2016;39:687–98.
81. Lemola S, Raikkonen K, Scheier MF, et al. Sleep quantity, quality, and
optimism in children. J Sleep Res 2011;20:12–20.
82. Jiang X, Hardy LL, Bauer LA, et al. Sleep duration, schedule and quality
among urban Chinese children and adolescents: associations with routine
after-school activities. PLoS One 2015;10:e0115326.
83. Olds T, Maher C, Blunden S, Matricciani L. Normative data on the sleep habits
of Australian children and adolescents. Sleep 2010;33:1381–8.
84. Price AM, Quach J, Wake M, Bittman M, Hiscock H. Cross-sectional sleep
thresholds for optimal health and well-being in Australian 4 to 9-year-olds.
Sleep Med 2016;22:83–90.
85. Chugani HT, Phelps ME, Mazziotta JC. Positron emission tomography study of
human brain functional development. Ann Neurol 1987;22:487–97.
ACKNOWLEDGMENTS
The AASM acknowledges the following individuals for their participation and
contributions: Non-Participating Observers: Michael Twery, PhD, National Health,
Lung, Blood Institute, NIH, Bethesda, MD; and Joel Porquez, RST, RPSGT, CCSH,
American Association of Sleep Technologists. American Academy of Sleep Medicine
Staff: John Noel; Jonathan L. Heald, MA; and Sarah Hashmi, MBBS, MSc, MPH.
SUBMISSION & CORRESPONDENCE INFORMATION
Submitted for publication September, 2016
Accepted for publication September, 2016
Address correspondence to: Shalini Paruthi, MD, St. Luke’s Hospital, 232 S. Woods
Mill Road, St. Louis, MO 63017; Email: research@aasmnet.org
DISCLOSURE STATEMENT
Funding for this project was provided by the American Academy of Sleep Medicine,
and supported by the cooperative agreement number 1U50DP004930-03 from
the Centers for Disease Control and Prevention (CDC). Its contents are solely the
responsibility of the authors and do not necessarily represent the ofcial views of the
CDC. Dr. Maski has consulted for Medscape Inc. and has received research support
from Jazz Pharmaceuticals. Dr. Rosen has consulted as a medical advisor for Jazz
Pharmaceuticals. The other Consensus Conference Panel members have indicated
no nancial conicts of interest.

LITERATURE SEARCH TERMS
Category Search Term
Sleep Duration
Napping [All fields]
Sleep debt [All fields]
Short sleep [All fields]
Long sleep [All fields]
Sleep deprivation [All fields]
Insufficient sleep
syndrome
[All fields]
Excessive sleep [All fields]
Sleep curtailment [All fields]
Sleep length [All fields]
Sleep need [All fields]
Sleep duration [All fields]
Sleep deficiency [All fields]
Cancer
Neoplasms [MeSH terms]
Cardiovascular
Health
Cardiovascular
diseases
[MeSH terms]
Heart valves [MeSH terms]
Heart valve
diseases
[MeSH terms]
Blood pressure [MeSH terms]
Developmental
Health
Child Development
Disorders, Pervasive
[MeSH terms]
Academic
performance
[All fields]
Behavior [MeSH terms]
Psychology,
educational
[MeSH terms]
Personality [MeSH terms]
Learning [MeSH terms]
Attention [MeSH terms]
School start time [All fields]
Neuropsychological
tests
[MeSH terms]
Neuropsycholo* [All fields]
Neurocognitive [All fields]
Neurobehavioral [All fields]
Emotional regulation [All fields]
Language [MeSH terms]
Socialization [MeSH terms]
Category Search Term
Human
Performance
Function [All fields]
Activities of daily
living
[MeSH terms]
Alertness [All fields]
Cognition [MeSH terms]
Patient safety [All fields]
Patient harms [All fields]
Accidents [MeSH terms]
Accident proneness [MeSH terms]
Fatigue [MeSH terms]
Vigilance [All fields]
Psychomotor
performance
[MeSH terms]
Reaction [All fields]
Comprehension [MeSH terms]
Confusion [MeSH terms]
Impairment [All fields]
Sleepiness
NOT sleep disorders
[All fields]
Sleep satisfaction [All fields]
Achievement [MeSH terms]
Athletic performance [MeSH terms]
Automobile driving [MeSH terms]
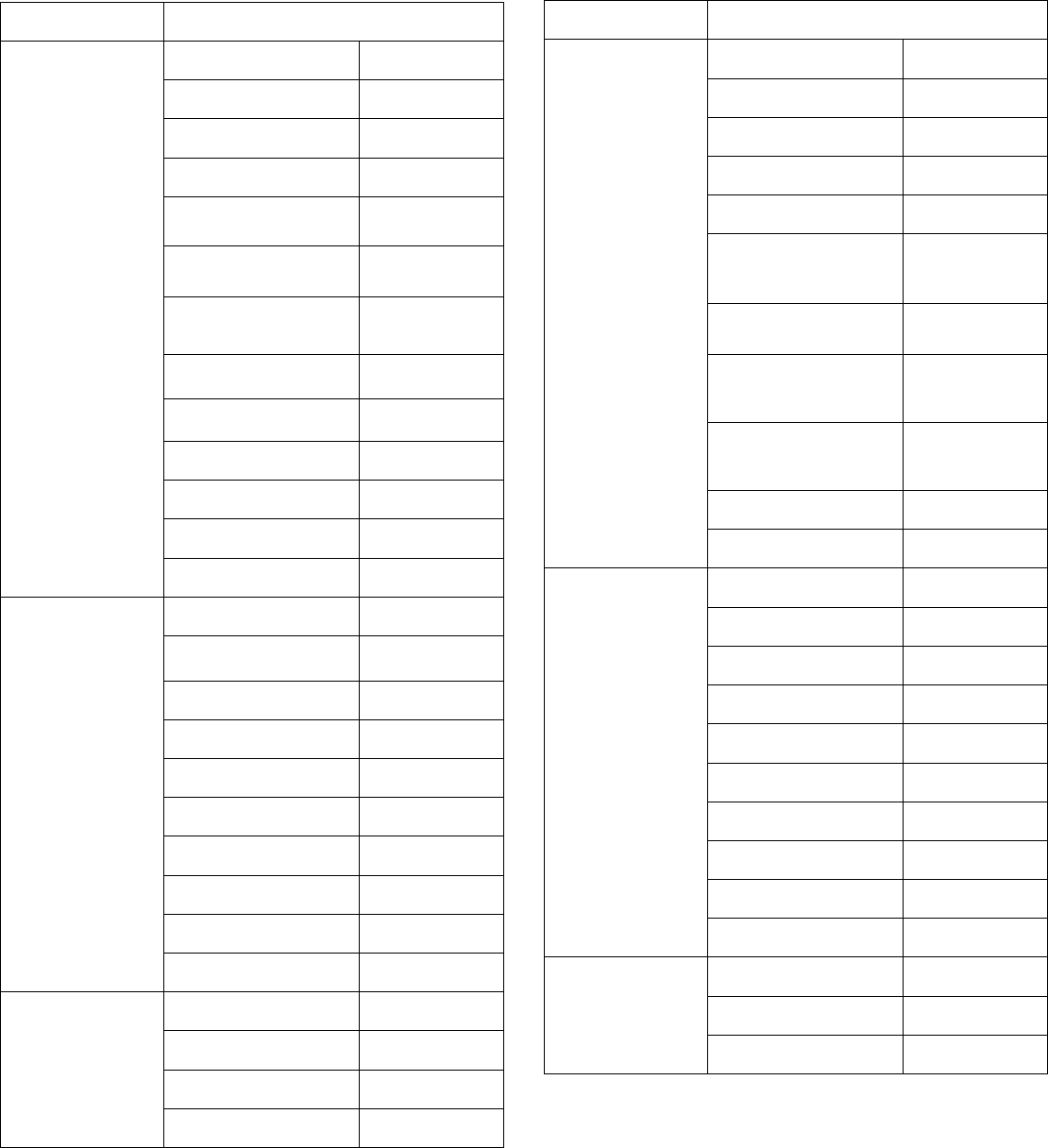
Category Search Term
General Health
Epidemiology [MeSH terms]
Prevention medicine [MeSH terms]
Emergencies [All fields]
Endemic diseases [All fields]
Environmental
medicine
[All fields]
Environmental
microbiology
[MeSH terms]
Disease
transmission,
infectious
[MeSH terms]
Environmental
pollution
[MeSH terms]
Public health
practice
[MeSH terms]
Wellness [All fields]
Well-being [All fields]
Quality of life [MeSH terms]
Wounds and Injuries [MeSH terms]
Immunological
Health
Inflammation [MeSH terms]
Autoimmune
disease
[MeSH terms]
Cytokines [MeSH terms]
Leukocytes [MeSH terms]
Phagocytes [MeSH terms]
Immunoproteins [MeSH terms]
Vaccination [MeSH terms]
Asthma [MeSH terms]
Common cold [MeSH terms]
Infection [MeSH terms]
Longevity
Death [MeSH terms]
Survival [MeSH terms]
Vital statistics [MeSH terms]
Suicide [MeSH terms]
Category Search Term
Mental Health
Mental Health [MeSH terms]
Depression [MeSH terms]
Psychiatry [MeSH terms]
Anxiety disorders [MeSH terms]
Mood disorders [MeSH terms]
Schizophrenia and
disorders with
psychotic features
[MeSH terms]
Substance-related
disorders
[MeSH terms]
Mental Disorders
Diagnosed in
Childhood
[MeSH terms]
Attention Deficit and
Disruptive Behavior
Disorders
[MeSH terms]
Eating disorders [MeSH terms]
Emotions [MeSH terms]
Metabolic Health
Metabolism [MeSH terms]
Body weight [MeSH terms]
Metabolic disease [MeSH terms]
Insulin [MeSH terms]
Orexins [MeSH terms]
Ghrelin [MeSH terms]
Adipokines [MeSH terms]
Waist-hip ratio [MeSH terms]
Thyroid gland [MeSH terms]
Pediatric obesity [MeSH terms]
Pain
Pain [MeSH terms]
Nociception [MeSH terms]
Rheumatic diseases [MeSH terms]
REFERENCE LIST OF FINAL EVIDENCE
Cardiovascular Health
Au CT, Ho CK, Wing YK, Lam HS, Li AM. Acute and chronic
effects of sleep duration on blood pressure. Pediatrics.
2014 Jan;133(1):e64-72.
Azadbakht L, Kelishadi R, Khodarahmi M, Qorbani M,
Heshmat R, Motlagh ME, Taslimi M, Ardalan G. The
association of sleep duration and cardiometabolic risk
factors in a national sample of children and adolescents:
the CASPIAN III study. Nutrition. 2013 Sep;29(9):1133-41.
Berentzen NE, Smit HA, Bekkers MB, Brunekreef B,
Koppelman GH, De Jongste JC, Kerkhof M, Van Rossem
L, Wijga AH. Time in bed, sleep quality and associations
with cardiometabolic markers in children: the Prevention
and Incidence of Asthma and Mite Allergy birth cohort
study. J Sleep Res. 2014 Feb;23(1):3-12.
Countryman AJ, Saab PG, Llabre MM, Penedo FJ, McCalla
JR, Schneiderman N. Cardiometabolic risk in adolescents:
associations with physical activity, fitness, and sleep. Ann
Behav Med. 2013 Feb;45(1):121-31.
Guo X, Zheng L, Li Y, Yu S, Liu S, Zhou X, Zhang X, Sun Z,
Wang R, Sun Y. Association between sleep duration and
hypertension among Chinese children and adolescents.
Clin Cardiol. 2011 Dec;34(12):774-81.
Javaheri S, Storfer-Isser A, Rosen CL, Redline S. Sleep
quality and elevated blood pressure in adolescents.
Circulation. 2008 Sep 2;118(10):1034-40.
Kuciene R, Dulskiene V. Associations of short sleep duration
with prehypertension and hypertension among Lithuanian
children and adolescents: a cross-sectional study. BMC
Public Health. 2014 Mar 15;14:255.
Lee JA, Park HS. Relation between sleep duration,
overweight, and metabolic syndrome in Korean
adolescents. Nutr Metab Cardiovasc Dis. 2014
Jan;24(1):65-71.
Lehto R, Ray C, Lahti-Koski M, Roos E. Health behaviors,
waist circumference and waist-to-height ratio in children.
Eur J Clin Nutr. 2011 Jul;65(7):841-8.
Mahler B, Kamperis K, Schroeder M, Frøkiær J, Djurhuus
JC, Rittig S. Sleep deprivation induces excess diuresis
and natriuresis in healthy children. Am J Physiol Renal
Physiol. 2012 Jan 15;302(2):F236-43.
Martikainen S, Pesonen AK, Feldt K, Jones A, Lahti J,
Pyhälä R, Heinonen K, Kajantie E, Eriksson J, Räikkönen
K. Poor sleep and cardiovascular function in children.
Hypertension. 2011 Jul;58(1):16-21.
Martinez-Gomez D, Eisenmann JC, Gomez-Martinez S, Hill
EE, Zapatera B, Veiga OL, Marcos A; AFINOS Study
Group. Sleep duration and emerging cardiometabolic risk
markers in adolescents. The AFINOS study. Sleep Med.
2011 Dec;12(10):997-1002.
Meininger JC, Gallagher MR, Eissa MA, Nguyen TQ, Chan
W. Sleep duration and its association with ambulatory
blood pressure in a school-based, diverse sample of
adolescents. Am J Hypertens. 2014 Jul;27(7):948-55.
Paciência I, Barros H, Araújo J, Ramos E. Association
between sleep duration and blood pressure in
adolescents. Hypertens Res. 2013 Aug;36(8):747-52.
Peach H, Gaultney JF, Reeve CL. Sleep characteristics,
body mass index, and risk for hypertension in young
adolescents. J Youth Adolesc. 2015 Feb;44(2):271-84.
Rey-López JP, de Carvalho HB, de Moraes AC, Ruiz JR,
Sjöström M, Marcos A, Polito A, Gottrand F, Manios Y,
Kafatos A, Molnar D, Widhalm K, De Henauw S, Moreno
LA; HELENA study. Sleep time and cardiovascular risk
factors in adolescents: the HELENA (Healthy Lifestyle in
Europe by Nutrition in Adolescence) study. Sleep Med.
2014 Jan;15(1):104-10.
Sampei M, Murata K, Dakeishi M, Wood DC. Cardiac
autonomic hypofunction in preschool children with short
nocturnal sleep. Tohoku J Exp Med. 2006 Mar;208(3):235-
42.
Sampei M, Dakeishi M, Wood DC, Murata K. Impact of total
sleep duration on blood pressure in preschool children.
Biomed Res. 2006 Jun;27(3):111-5.
Sung V, Beebe DW, Vandyke R, Fenchel MC, Crimmins NA,
Kirk S, Hiscock H, Amin R, Wake M. Does sleep duration
predict metabolic risk in obese adolescents attending
tertiary services? A cross-sectional study. Sleep. 2011 Jul
1;34(7):891-8.
Wells JC, Hallal PC, Reichert FF, Menezes AM, Araújo CL,
Victora CG. Sleep patterns and television viewing in
relation to obesity and blood pressure: evidence from an
adolescent Brazilian birth cohort. Int J Obes (Lond). 2008
Jul;32(7):1042-9.
Developmental Health
Abe T, Hagihara A, Nobutomo K. Sleep patterns and
impulse control among Japanese junior high school
students. J Adolesc. 2010 Oct;33(5):633-41.
Adolescent Sleep Working Group; Committee on
Adolescence; Council on School Health. School start
times for adolescents. Pediatrics. 2014 Sep;134(3):642-9.
Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk
factors for childhood overweight: a prospective study from
birth to 9.5 years. J Pediatr. 2004 Jul;145(1):20-5. Erratum
in: J Pediatr. 2004 Sep;145(3):424.
Aishworiya R, Chan P, Kiing J, Chong SC, Laino AG, Tay
SKh. Sleep behaviour in a sample of preschool children in
Singapore. Ann Acad Med Singapore. 2012 Mar;41(3):99-
104.
Al-Hazzaa HM, Musaiger AO, Abahussain NA, Al-Sobayel
HI, Qahwaji DM. Lifestyle correlates of self-reported sleep
duration among Saudi adolescents: a multicentre school-
based cross-sectional study. Child Care Health Dev. 2014
Jul;40(4):533-42.
Anderson B, Storfer-Isser A, Taylor HG, Rosen CL, Redline
S. Associations of executive function with sleepiness and
sleep duration in adolescents. Pediatrics. 2009
Apr;123(4):e701-7.
Androutsos O, Moschonis G, Mavrogianni C, Roma-
Giannikou E, Chrousos GP, Kanaka-Gantenbein C,
Manios Y. Identification of lifestyle patterns, including
sleep deprivation, associated with insulin resistance in
children: the Healthy Growth Study. Eur J Clin Nutr. 2014
Mar;68(3):344-9.
Anuntaseree W, Mo-suwan L, Vasiknanonte P, Kuasirikul S,
Ma-a-lee A, Choprapawan C. Night waking in Thai infants
at 3 months of age: association between parental
practices and infant sleep. Sleep Med. 2008 Jul;9(5):564-
71.
Appelhans BM, Fitzpatrick SL, Li H, Cail V, Waring ME,
Schneider KL, Whited MC, Busch AM, Pagoto SL. The
home environment and childhood obesity in low-income
households: indirect effects via sleep duration and screen
time. BMC Public Health. 2014 Nov 9;14:1160.
Arakawa M, Taira K, Tanaka H, Yamakawa K, Toguchi H,
Kadekaru H, Yamamoto Y, Uezu E, Shirakawa S. A
survey of junior high school students' sleep habit and
lifestyle in Okinawa. Psychiatry Clin Neurosci. 2001
Jun;55(3):211-2.
Aronen ET, Paavonen EJ, Fällberg M, Soininen M, Törrönen
J. Sleep and psychiatric symptoms in school-age children.
J Am Acad Child Adolesc Psychiatry. 2000 Apr;39(4):502-
8.
Arora T, Taheri S. Associations among late chronotype,
body mass index and dietary behaviors in young
adolescents. Int J Obes (Lond). 2015 Jan;39(1):39-44.
Arora T, Hosseini-Araghi M, Bishop J, Yao GL, Thomas GN,
Taheri S. The complexity of obesity in U.K. adolescents:
relationships with quantity and type of technology, sleep
duration and quality, academic performance and
aspiration. Pediatr Obes. 2013 Oct;8(5):358-66.
Asaka Y, Takada S. Activity-based assessment of the sleep
behaviors of VLBW preterm infants and full-term infants at
around 12 months of age. Brain Dev. 2010 Feb;32(2):150-
5.
Asarnow LD, McGlinchey E, Harvey AG. The effects of
bedtime and sleep duration on academic and emotional
outcomes in a nationally representative sample of
adolescents. J Adolesc Health. 2014 Mar;54(3):350-6.
Astill RG, Van der Heijden KB, Van Ijzendoorn MH, Van
Someren EJ. Sleep, cognition, and behavioral problems in
school-age children: a century of research meta-analyzed.
Psychol Bull. 2012 Nov;138(6):1109-38.
BaHammam A, Bin Saeed A, Al-Faris E, Shaikh S. Sleep
duration and its correlates in a sample of Saudi
elementary school children. Singapore Med J. 2006
Oct;47(10):875-81.
Ball GD, Lenk JM, Barbarich BN, Plotnikoff RC, Fishburne
GJ, Mackenzie KA, Willows ND. Overweight children and
adolescents referred for weight management: are they
meeting lifestyle behaviour recommendations? Appl
Physiol Nutr Metab. 2008 Oct;33(5):936-45.
Barnes JC, Meldrum RC. The impact of sleep duration on
adolescent development: a genetically informed analysis
of identical twin pairs. J Youth Adolesc. 2015
Feb;44(2):489-506.
Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW.
Sleep restriction worsens mood and emotion regulation in
adolescents. J Child Psychol Psychiatry. 2014;55(2):180-
90.
Beebe DW, Simon S, Summer S, Hemmer S, Strotman D,
Dolan LM. Dietary intake following experimentally
restricted sleep in adolescents. Sleep. 2013 Jun
1;36(6):827-34.
Beebe DW, Ris MD, Kramer ME, Long E, Amin R. The
association between sleep disordered breathing,
academic grades, and cognitive and behavioral
functioning among overweight subjects during middle to
late childhood. Sleep. 2010 Nov;33(11):1447-56.
Beebe DW, Rose D, Amin R. Attention, learning, and arousal
of experimentally sleep-restricted adolescents in a
simulated classroom. J Adolesc Health. 2010
Nov;47(5):523-5.
Beebe DW, Fallone G, Godiwala N, Flanigan M, Martin D,
Schaffner L, Amin R. Feasibility and behavioral effects of
an at-home multi-night sleep restriction protocol for
adolescents. J Child Psychol Psychiatry. 2008
Sep;49(9):915-23.
Bel S, Michels N, De Vriendt T, Patterson E, Cuenca-García
M, Diethelm K, Gutin B, Grammatikaki E, Manios Y,
Leclercq C, Ortega FB, Moreno LA, Gottrand F, Gonzalez-
Gross M, Widhalm K, Kafatos A, Garaulet M, Molnar D,
Kaufman JM, Gilbert CC, Hallström L, Sjöström M, et al.
Association between self-reported sleep duration and
dietary quality in European adolescents. Br J Nutr. 2013
Sep 14;110(5):949-59.
Berger RH, Miller AL, Seifer R, Cares SR, LeBourgeois MK.
Acute sleep restriction effects on emotion responses in 30-
to 36-month-old children. J Sleep Res. 2012
Jun;21(3):235-46.
Bertelle V, Sevestre A, Laou-Hap K, Nagahapitiye MC, Sizun
J. Sleep in the neonatal intensive care unit. J Perinat
Neonatal Nurs. 2007 Apr-Jun;21(2):140-8; quiz 149-50.
Review.
Bertelle V, Mabin D, Adrien J, Sizun J. Sleep of preterm
neonates under developmental care or regular
environmental conditions. Early Hum Dev. 2005
Jul;81(7):595-600.
Bibiloni Mdel M, Martinez E, Llull R, Juarez MD, Pons A, Tur
JA. Prevalence and risk factors for obesity in Balearic
Islands adolescents. Br J Nutr. 2010 Jan;103(1):99-106.
Biggs SN, Lushington K, van den Heuvel CJ, Martin AJ,
Kennedy JD. Inconsistent sleep schedules and daytime
behavioral difficulties in school-aged children. Sleep Med.
2011 Sep;12(8):780-6.
Bruni O, Baumgartner E, Sette S, Ancona M, Caso G, Di
Cosimo ME, Mannini A, Ometto M, Pasquini A, Ulliana A,
Ferri R. Longitudinal study of sleep behavior in normal
infants during the first year of life. J Clin Sleep Med. 2014
Oct 15;10(10):1119-27.
Bruni O, Russo PM, Ferri R, Novelli L, Galli F, Guidetti V.
Relationships between headache and sleep in a non-
clinical population of children and adolescents. Sleep Med.
2008 Jul;9(5):542-8.
Buckhalt JA, El-Sheikh M, Keller P. Children's sleep and
cognitive functioning: race and socioeconomic status as
moderators of effects. Child Dev. 2007 Jan-Feb;78(1):213-
31.
Burt J, Dube L, Thibault L, Gruber R. Sleep and eating in
childhood: a potential behavioral mechanism underlying
the relationship between poor sleep and obesity. Sleep
Med. 2014 Jan;15(1):71-5.
Calamaro CJ, Park S, Mason TB, Marcus CL, Weaver TE,
Pack A, Ratcliffe SJ. Shortened sleep duration does not
predict obesity in adolescents. J Sleep Res. 2010
Dec;19(4):559-66
Calamaro CJ, Mason TB, Ratcliffe SJ. Adolescents living the
24/7 lifestyle: effects of caffeine and technology on sleep
duration and daytime functioning. Pediatrics. 2009
Jun;123(6):e1005-10.
Capaldi Ii VF, Handwerger K, Richardson E, Stroud LR.
Associations between sleep and cortisol responses to
stress in children and adolescents: a pilot study. Behav
Sleep Med. 2005;3(4):177-92.
Carskadon MA. Sleep's effects on cognition and learning in
adolescence. Prog Brain Res. 2011;190:137-43.
Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer
R. Adolescent sleep patterns, circadian timing, and
sleepiness at a transition to early school days. Sleep.
1998 Dec 15;21(8):871-81.
Carvalho Bos S, Gomes A, Clemente V, Marques M, Pereira
AT, Maia B, Soares MJ, Cabral AS, Macedo A, Gozal D,
Azevedo MH. Sleep and behavioral/emotional problems in
children: a population-based study. Sleep Med. 2009
Jan;10(1):66-74.
Cassoff J, Bhatti JA, Gruber R. The effect of sleep restriction
on neurobehavioural functioning in normally developing
children and adolescents: insights from the Attention,
Behaviour and Sleep Laboratory. Pathol Biol (Paris). 2014
Oct;62(5):319-31.
Chung KF, Cheung MM. Sleep-wake patterns and sleep
disturbance among Hong Kong Chinese adolescents.
Sleep. 2008 Feb;31(2):185-94.
Cicek B, Ozturk A, Mazicioglu MM, Elmali F, Turp N,
Kurtoglu S. The risk analysis of arm fat area in Turkish
children and adolescents. Ann Hum Biol. 2009 Jan-
Feb;36(1):28-37.
Cortesi F, Giannotti F, Sebastiani T, Vagnoni C, Marioni P.
Cosleeping versus solitary sleeping in children with
bedtime problems: child emotional problems and parental
distress. Behav Sleep Med. 2008;6(2):89-105
Countryman AJ, Saab PG, Llabre MM, Penedo FJ, McCalla
JR, Schneiderman N. Cardiometabolic risk in adolescents:
associations with physical activity, fitness, and sleep. Ann
Behav Med. 2013 Feb;45(1):121-31.
Crosby B, LeBourgeois MK, Harsh J. Racial differences in
reported napping and nocturnal sleep in 2- to 8-year-old
children. Pediatrics. 2005 Jan;115(1 Suppl):225-32.
Dahl RE. Biological, developmental, and neurobehavioral
factors relevant to adolescent driving risks. Am J Prev
Med. 2008 Sep;35(3 Suppl):S278-84.
Dahl RE, Lewin DS. Pathways to adolescent health sleep
regulation and behavior. J Adolesc Health. 2002 Dec;31(6
Suppl):175-84. Review.
Davis AL, Avis KT, Schwebel DC. The effects of acute sleep
restriction on adolescents' pedestrian safety in a virtual
environment. J Adolesc Health. 2013 Dec;53(6):785-90.
de Jong E, Stocks T, Visscher TL, HiraSing RA, Seidell JC,
Renders CM. Association between sleep duration and
overweight: the importance of parenting. Int J Obes
(Lond). 2012 Oct;36(10):1278-84
Dev DA, McBride BA, Fiese BH, Jones BL, Cho H; Behalf Of
The Strong Kids Research Team. Risk factors for
overweight/obesity in preschool children: an ecological
approach. Child Obes. 2013 Oct;9(5):399-408.
Dewald JF, Short MA, Gradisar M, Oort FJ, Meijer AM. The
Chronic Sleep Reduction Questionnaire (CSRQ): a cross-
cultural comparison and validation in Dutch and Australian
adolescents. J Sleep Res. 2012 Oct;21(5):584-94.
Dexter D, Bijwadia J, Schilling D, Applebaugh G. Sleep,
sleepiness and school start times: a preliminary study.
WMJ. 2003;102(1):44-6.
Do YK, Shin E, Bautista MA, Foo K. The associations
between self-reported sleep duration and adolescent
health outcomes: what is the role of time spent on Internet
use? Sleep Med. 2013 Feb;14(2):195-200.
Doane LD, Thurston EC. Associations among sleep, daily
experiences, and loneliness in adolescence: evidence of
moderating and bidirectional pathways. J Adolesc. 2014
Feb;37(2):145-54.
Dollman J, Ridley K, Olds T, Lowe E. Trends in the duration
of school-day sleep among 10- to 15-year-old South
Australians between 1985 and 2004. Acta Paediatr. 2007
Jul;96(7):1011-4.
Dorofaeff TF, Denny S. Sleep and adolescence. Do New
Zealand teenagers get enough? J Paediatr Child Health.
2006 Sep;42(9):515-20.
Duncan JS, Schofield G, Duncan EK, Rush EC. Risk factors
for excess body fatness in New Zealand children. Asia
Pac J Clin Nutr. 2008;17(1):138-47.
Eaton DK, McKnight-Eily LR, Lowry R, Perry GS, Presley-
Cantrell L, Croft JB. Prevalence of insufficient, borderline,
and optimal hours of sleep among high school students -
United States, 2007. J Adolesc Health. 2010
Apr;46(4):399-401.
El-Sheikh M, Buckhalt JA, Mark Cummings E, Keller P.
Sleep disruptions and emotional insecurity are pathways
of risk for children. J Child Psychol Psychiatry. 2007
Jan;48(1):88-96.
Elsenburg LK, Corpeleijn E, van Sluijs EM, Atkin AJ.
Clustering and correlates of multiple health behaviours in
9-10 year old children. PLoS One. 2014;9(6):e99498.
Ertan P, Yilmaz O, Caglayan M, Sogut A, Aslan S, Yuksel
H. Relationship of sleep quality and quality of life in
children with monosymptomatic enuresis. Child Care
Health Dev. 2009 Jul;35(4):469-74.
Escribano C, Díaz-Morales JF. Daily fluctuations in attention
at school considering starting time and chronotype: an
exploratory study. Chronobiol Int. 2014 Jul;31(6):761-9.
Fallone G, Acebo C, Seifer R, Carskadon MA. Experimental
restriction of sleep opportunity in children: effects on
teacher ratings. Sleep. 2005 Dec;28(12):1561-7.
Fallone G, Acebo C, Arnedt JT, Seifer R, Carskadon MA.
Effects of acute sleep restriction on behavior, sustained
attention, and response inhibition in children. Percept Mot
Skills. 2001 Aug;93(1):213-29.
Firouzi S, Poh BK, Ismail MN, Sadeghilar A. Sleep habits,
food intake, and physical activity levels in normal and
overweight and obese Malaysian children. Obes Res Clin
Pract. 2014 Jan-Feb;8(1):e70-8.
Fitzgerald CT, Messias E, Buysse DJ. Teen sleep and
suicidality: results from the youth risk behavior surveys of
2007 and 2009. J Clin Sleep Med. 2011 Aug 15;7(4):351-
6.
Fredriksen K, Rhodes J, Reddy R, Way N. Sleepless in
Chicago: tracking the effects of adolescent sleep loss
during the middle school years. Child Dev. 2004 Jan-
Feb;75(1):84-95.
Fukuda K, Ishihara K. Routine evening naps and night-time
sleep patterns in junior high and high school students.
Psychiatry Clin Neurosci. 2002 Jun;56(3):229-30.
Gaina A, Sekine M, Hamanishi S, Chen X, Wang H,
Yamagami T, Kagamimori S. Daytime sleepiness and
associated factors in Japanese school children. J Pediatr.
2007 Nov;151(5):518-22, 522.e1-4.
Garaulet M, Ortega FB, Ruiz JR, Rey-López JP, Béghin L,
Manios Y, Cuenca-García M, Plada M, Diethelm K,
Kafatos A, Molnár D, Al-Tahan J, Moreno LA. Short sleep
duration is associated with increased obesity markers in
European adolescents: effect of physical activity and
dietary habits. The HELENA study. Int J Obes (Lond).
2011 Oct;35(10):1308-17.
Garmy P, Nyberg P, Jakobsson U. Sleep and television and
computer habits of Swedish school-age children. J Sch
Nurs. 2012 Dec;28(6):469-76.
Gau SS, Shang CY, Merikangas KR, Chiu YN, Soong WT,
Cheng AT. Association between morningness-
eveningness and behavioral/emotional problems among
adolescents. J Biol Rhythms. 2007 Jun;22(3):268-74.
Geiger A, Achermann P, Jenni OG. Association between
sleep duration and intelligence scores in healthy children.
Dev Psychol. 2010 Jul;46(4):949-54.
Giannotti F, Cortesi F, Cerquiglini A, Miraglia D, Vagnoni C,
Sebastiani T, Bernabei P. An investigation of sleep
characteristics, EEG abnormalities and epilepsy in
developmentally regressed and non-regressed children
with autism. J Autism Dev Disord. 2008 Nov;38(10):1888-
97.
Gibson ES, Powles AC, Thabane L, O'Brien S, Molnar DS,
Trajanovic N, Ogilvie R, Shapiro C, Yan M, Chilcott-
Tanser L. Sleepiness" is serious in adolescence: two
surveys of 3235 Canadian students." BMC Public Health.
2006 May 2;6:116.
Golley RK, Maher CA, Matricciani L, Olds TS. Sleep duration
or bedtime? Exploring the association between sleep
timing behaviour, diet and BMI in children and
adolescents. Int J Obes (Lond). 2013 Apr;37(4):546-51.
Gruber R, Cassoff J, Frenette S, Wiebe S, Carrier J. Impact
of sleep extension and restriction on children's emotional
lability and impulsivity. Pediatrics. 2012 Nov;130(5):e1155-
61.
Gruber R, Wiebe S, Montecalvo L, Brunetti B, Amsel R,
Carrier J. Impact of sleep restriction on neurobehavioral
functioning of children with attention deficit hyperactivity
disorder. Sleep. 2011 Mar 1;34(3):315-23.
Gruber R, Laviolette R, Deluca P, Monson E, Cornish K,
Carrier J. Short sleep duration is associated with poor
performance on IQ measures in healthy school-age
children. Sleep Med. 2010 Mar;11(3):289-94.
Guo X, Zheng L, Li Y, Yu S, Sun G, Yang H, Zhou X, Zhang
X, Sun Z, Sun Y. Differences in lifestyle behaviors, dietary
habits, and familial factors among normal-weight,
overweight, and obese Chinese children and adolescents.
Int J Behav Nutr Phys Act. 2012 Oct 2;9:120.
Gössel-Symank R, Grimmer I, Korte J, Siegmund R.
Actigraphic monitoring of the activity-rest behavior of
preterm and full-term infants at 20 months of age.
Chronobiol Int. 2004 Jul;21(4-5):661-71.
Hagenauer MH, Perryman JI, Lee TM, Carskadon MA.
Adolescent changes in the homeostatic and circadian
regulation of sleep. Dev Neurosci. 2009;31(4):276-84.
Haines J, McDonald J, O'Brien A, Sherry B, Bottino CJ,
Schmidt ME, Taveras EM. Healthy Habits, Happy Homes:
randomized trial to improve household routines for obesity
prevention among preschool-aged children. JAMA Pediatr.
2013 Nov;167(11):1072-9.
Harrington SA. Relationships of objectively measured
physical activity and sleep with BMI and academic
outcomes in 8-year-old children. Appl Nurs Res. 2013
May;26(2):63-70.
Hart CN, Carskadon MA, Considine RV, Fava JL, Lawton J,
Raynor HA, Jelalian E, Owens J, Wing R. Changes in
children's sleep duration on food intake, weight, and leptin.
Pediatrics. 2013 Dec;132(6):e1473-80.
Hiscock H, Sciberras E, Mensah F, Gerner B, Efron D,
Khano S, Oberklaid F. Impact of a behavioural sleep
intervention on symptoms and sleep in children with
attention deficit hyperactivity disorder, and parental mental
health: randomised controlled trial. BMJ. 2015 Jan
20;350:h68.
Hjorth MF, Chaput JP, Ritz C, Dalskov SM, Andersen R,
Astrup A, Tetens I, Michaelsen KF, Sjödin A. Fatness
predicts decreased physical activity and increased
sedentary time, but not vice versa: support from a
longitudinal study in 8- to 11-year-old children. Int J Obes
(Lond). 2014 Jul;38(7):959-65.
Hjorth MF, Quist JS, Andersen R, Michaelsen KF, Tetens I,
Astrup A, Chaput JP, Sjödin A. Change in sleep duration
and proposed dietary risk factors for obesity in Danish
school children. Pediatr Obes. 2014 Dec;9(6):e156-9.
Hodge D, Carollo TM, Lewin M, Hoffman CD, Sweeney DP.
Sleep patterns in children with and without autism
spectrum disorders: developmental comparisons. Res Dev
Disabil. 2014 Jul;35(7):1631-8.
Holley S, Hill CM, Stevenson J. An hour less sleep is a risk
factor for childhood conduct problems. Child Care Health
Dev. 2011 Jul;37(4):563-70.
Holm SM, Forbes EE, Ryan ND, Phillips ML, Tarr JA, Dahl
RE. Reward-related brain function and sleep in pre/early
pubertal and mid/late pubertal adolescents. J Adolesc
Health. 2009 Oct;45(4):326-34.
Honomichl RD, Goodlin-Jones BL, Burnham M, Gaylor E,
Anders TF. Sleep patterns of children with pervasive
developmental disorders. J Autism Dev Disord. 2002
Dec;32(6):553-61.
Humphreys JS, Gringras P, Blair PS, Scott N, Henderson J,
Fleming PJ, Emond AM. Sleep patterns in children with
autistic spectrum disorders: a prospective cohort study.
Arch Dis Child. 2014 Feb;99(2):114-8.
Hupbach A, Gomez RL, Bootzin RR, Nadel L. Nap-
dependent learning in infants. Dev Sci. 2009
Nov;12(6):1007-12.
Hysing M, Harvey AG, Torgersen L, Ystrom E, Reichborn-
Kjennerud T, Sivertsen B. Trajectories and predictors of
nocturnal awakenings and sleep duration in infants. J Dev
Behav Pediatr. 2014 Jun;35(5):309-16.
Ikeda M, Kaneita Y, Kondo S, Itani O, Ohida T.
Epidemiological study of sleep habits among four-and-a-
half-year-old children in Japan. Sleep Med. 2012
Aug;13(7):787-94.
Jang SI, Lee KS, Park EC. Relationship between current
sleep duration and past suicidal ideation or attempt among
Korean adolescents. J Prev Med Public Health. 2013
Nov;46(6):329-35.
Jarrin DC, McGrath JJ, Drake CL. Beyond sleep duration:
distinct sleep dimensions are associated with obesity in
children and adolescents. Int J Obes (Lond). 2013
Apr;37(4):552-8.
Javaheri S, Storfer-Isser A, Rosen CL, Redline S.
Association of short and long sleep durations with insulin
sensitivity in adolescents. J Pediatr. 2011 Apr;158(4):617-
23.
Jiang X, Hardy LL, Baur LA, Ding D, Wang L, Shi H. Sleep
duration, schedule and quality among urban Chinese
children and adolescents: associations with routine after-
school activities. PLoS One. 2015;10(1):e0115326.
Kang SG, Lee YJ, Kim SJ, Lim W, Lee HJ, Park YM, Cho IH,
Cho SJ, Hong JP. Weekend catch-up sleep is
independently associated with suicide attempts and self-
injury in Korean adolescents. Compr Psychiatry. 2014
Feb;55(2):319-25.
Keller PS, El-Sheikh M, Buckhalt JA. Children's attachment
to parents and their academic functioning: sleep
disruptions as moderators of effects. J Dev Behav Pediatr.
2008 Dec;29(6):441-9.
Kelly RJ, El-Sheikh M. Reciprocal relations between
children's sleep and their adjustment over time. Dev
Psychol. 2014 Apr;50(4):1137-47.
Kim HS, Ham OK, Kim JW, Park JY. Association between
sleep duration and psychological health in overweight and
obese children in Korea. Nurs Health Sci. 2012
Jun;14(2):238-43.
Kirjavainen J, Lehtonen L, Kirjavainen T, Kero P; 24-Hour
Ambulatory Sleep Polygraphy study. Sleep of excessively
crying infants: a 24-Hour Ambulatory Sleep Polygraphy
study. Pediatrics. 2004 Sep;114(3):592-600.
Kjeldsen JS, Hjorth MF, Andersen R, Michaelsen KF, Tetens
I, Astrup A, Chaput JP, Sjödin A. Short sleep duration and
large variability in sleep duration are independently
associated with dietary risk factors for obesity in Danish
school children. Int J Obes (Lond). 2014 Jan;38(1):32-9.
Kleiser C, Schaffrath Rosario A, Mensink GB, Prinz-
Langenohl R, Kurth BM. Potential determinants of obesity
among children and adolescents in Germany: results from
the cross-sectional KiGGS Study. BMC Public Health.
2009 Feb 2;9:46.
Klingenberg L, Chaput JP, Holmbäck U, Jennum P, Astrup
A, Sjödin A. Sleep restriction is not associated with a
positive energy balance in adolescent boys. Am J Clin
Nutr. 2012 Aug;96(2):240-8.
Kohyama J, Shiiki T, Ohinata-Sugimoto J, Hasegawa T.
Potentially harmful sleep habits of 3-year-old children in
Japan. J Dev Behav Pediatr. 2002 Apr;23(2):67-70.
Komada Y, Abe T, Okajima I, Asaoka S, Matsuura N, Usui
A, Shirakawa S, Inoue Y. Short sleep duration and
irregular bedtime are associated with increased behavioral
problems among Japanese preschool-age children.
Tohoku J Exp Med. 2011;224(2):127-36.
Kopasz M, Loessl B, Valerius G, Koenig E, Matthaeas N,
Hornyak M, Kloepfer C, Nissen C, Riemann D,
Voderholzer U. No persisting effect of partial sleep
curtailment on cognitive performance and declarative
memory recall in adolescents. J Sleep Res. 2010 Mar;19(1
Pt 1):71-9.
Kopasz M, Loessl B, Hornyak M, Riemann D, Nissen C,
Piosczyk H, Voderholzer U. Sleep and memory in healthy
children and adolescents - a critical review. Sleep Med
Rev. 2010 Jun;14(3):167-77.
Kostyun RO, Milewski MD, Hafeez I. Sleep disturbance and
neurocognitive function during the recovery from a sport-
related concussion in adolescents. Am J Sports Med.
2015 Mar;43(3):633-40.
Kouros CD, El-Sheikh M. Daily mood and sleep: reciprocal
relations and links with adjustment problems. J Sleep Res.
2015 Feb;24(1):24-31.
Kubiszewski V, Fontaine R, Potard C, Gimenes G. Bullying,
sleep/wake patterns and subjective sleep disorders:
findings from a cross-sectional survey. Chronobiol Int.
2014 May;31(4):542-53.
Kuciene R, Dulskiene V. Associations of short sleep duration
with prehypertension and hypertension among Lithuanian
children and adolescents: a cross-sectional study. BMC
Public Health. 2014 Mar 15;14:255.
Kuriyan R, Thomas T, Sumithra S, Lokesh DP, Sheth NR,
Joy R, Bhat S, Kurpad AV. Potential factors related to
waist circumference in urban South Indian children. Indian
Pediatr. 2012 Feb;49(2):124-8.
Kuriyan R, Bhat S, Thomas T, Vaz M, Kurpad AV. Television
viewing and sleep are associated with overweight among
urban and semi-urban South Indian children. Nutr J. 2007
Sep 20;6:25.
Kwon JA, Lee M, Yoo KB, Park EC. Does the duration and
time of sleep increase the risk of allergic rhinitis? Results
of the 6-year nationwide Korea youth risk behavior web-
based survey. PLoS One. 2013;8(8):e72507.
Lam JC, Mahone EM, Mason T, Scharf SM. The effects of
napping on cognitive function in preschoolers. J Dev
Behav Pediatr. 2011 Feb-Mar;32(2):90-7.
Lazaratou H, Dikeos DG, Anagnostopoulos DC, Sbokou O,
Soldatos CR. Sleep problems in adolescence. A study of
senior high school students in Greece. Eur Child Adolesc
Psychiatry. 2005 Jul;14(4):237-43.
Lee YJ, Cho SJ, Cho IH, Kim SJ. Insufficient sleep and
suicidality in adolescents. Sleep. 2012 Apr 1;35(4):455-60.
Lehto JE, Uusitalo-Malmivaara L. Sleep-related factors:
associations with poor attention and depressive
symptoms. Child Care Health Dev. 2014 May;40(3):419-
25.
Lehto R, Ray C, Lahti-Koski M, Roos E. Health behaviors,
waist circumference and waist-to-height ratio in children.
Eur J Clin Nutr. 2011 Jul;65(7):841-8.
Lemola S, Schwarz B, Siffert A. Interparental conflict and
early adolescents' aggression: is irregular sleep a
vulnerability factor? J Adolesc. 2012 Feb;35(1):97-105..
Lemola S, Räikkönen K, Scheier MF, Matthews KA,
Pesonen AK, Heinonen K, Lahti J, Komsi N, Paavonen JE,
Kajantie E. Sleep quantity, quality and optimism in
children. J Sleep Res. 2011 Mar;20(1 Pt 1):12-20.
Lewandowski AS, Palermo TM, De la Motte S, Fu R.
Temporal daily associations between pain and sleep in
adolescents with chronic pain versus healthy adolescents.
Pain. 2010 Oct;151(1):220-5.
Li S, Arguelles L, Jiang F, Chen W, Jin X, Yan C, Tian Y,
Hong X, Qian C, Zhang J, Wang X, Shen X. Sleep, school
performance, and a school-based intervention among
school-aged children: a sleep series study in China. PLoS
One. 2013 Jul 10;8(7):e67928.
Li Y, Jin H, Owens JA, Hu C. The association between sleep
and injury among school-aged children in rural China: a
case-control study. Sleep Med. 2008 Jan;9(2):142-8.
Lin WH, Yi CC. Unhealthy sleep practices, conduct
problems, and daytime functioning during adolescence. J
Youth Adolesc. 2015 Feb;44(2):431-46.
Liu X, Hubbard JA, Fabes RA, Adam JB. Sleep disturbances
and correlates of children with autism spectrum disorders.
Child Psychiatry Hum Dev. 2006 Winter;37(2):179-91.
Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004
Nov 1;27(7):1351-8.
Liu X, Uchiyama M, Okawa M, Kurita H. Prevalence and
correlates of self-reported sleep problems among Chinese
adolescents. Sleep. 2000 Feb 1;23(1):27-34.
Loessl B, Valerius G, Kopasz M, Hornyak M, Riemann D,
Voderholzer U. Are adolescents chronically sleep-
deprived? An investigation of sleep habits of adolescents
in the Southwest of Germany. Child Care Health Dev.
2008 Sep;34(5):549-56.
Lytle LA, Pasch KE, Farbakhsh K. The relationship between
sleep and weight in a sample of adolescents. Obesity
(Silver Spring). 2011 Feb;19(2):324-31.
Magee CA, Gordon R, Caputi P. Distinct developmental
trends in sleep duration during early childhood. Pediatrics.
2014 Jun;133(6):e1561-7.
Mak KK, Lee SL, Ho SY, Lo WS, Lam TH. Sleep and
academic performance in Hong Kong adolescents. J Sch
Health. 2012 Nov;82(11):522-7.
Malow BA, Marzec ML, McGrew SG, Wang L, Henderson
LM, Stone WL. Characterizing sleep in children with
autism spectrum disorders: a multidimensional approach.
Sleep. 2006 Dec;29(12):1563-71.
Martinez-Gomez D, Eisenmann JC, Gomez-Martinez S, Hill
EE, Zapatera B, Veiga OL, Marcos A; AFINOS Study
Group. Sleep duration and emerging cardiometabolic risk
markers in adolescents. The AFINOS study. Sleep Med.
2011 Dec;12(10):997-1002.
Martinez-Gomez D, Moreno LA, Romeo J, Rey-López P,
Castillo R, Cabero MJ, Vicente-Rodriguez G, Gutiérrez A,
Veiga OL. Combined influence of lifestyle risk factors on
body fat in Spanish adolescents--the Avena study. Obes
Facts. 2011;4(2):105-11.
Maski KP, Kothare SV. Sleep deprivation and
neurobehavioral functioning in children. Int J
Psychophysiol. 2013 Aug;89(2):259-64.
Matamura M, Tochigi M, Usami S, Yonehara H, Fukushima
M, Nishida A, Togo F, Sasaki T. Associations between
sleep habits and mental health status and suicidality in a
longitudinal survey of monozygotic twin adolescents. J
Sleep Res. 2014 Jun;23(3):290-4.
Matsushita M, Koyama A, Ushijima H, Mikami A, Katsumata
Y, Kikuchi Y, Ichimi N, Jono T, Fujise N, Ikeda M. Sleep
duration and its association with sleepiness and
depression in ronin-sei" preparatory school students."
Asian J Psychiatr. 2014 Jun;9:61-6.
McDermott BM, Mamun AA, Najman JM, Williams GM,
O'callaghan MJ, Bor W. Preschool children perceived by
mothers as irregular eaters: physical and psychosocial
predictors from a birth cohort study. J Dev Behav Pediatr.
2008 Jun;29(3):197-205.
Mcneil J, Tremblay MS, Leduc G, Boyer C, Bélanger P,
Leblanc AG, Borghese MM, Chaput JP. Objectively-
measured sleep and its association with adiposity and
physical activity in a sample of Canadian children. J Sleep
Res. 2015 Apr;24(2):131-9.
Meijer AM. Chronic sleep reduction, functioning at school
and school achievement in preadolescents. J Sleep Res.
2008 Dec;17(4):395-405. Erratum in: J Sleep Res. 2009
Mar;18(1):144.
Meininger JC, Gallagher MR, Eissa MA, Nguyen TQ, Chan
W. Sleep duration and its association with ambulatory
blood pressure in a school-based, diverse sample of
adolescents. Am J Hypertens. 2014 Jul;27(7):948-55.
Meldrum RC, Barnes JC, Hay C. Sleep deprivation, low self-
control, and delinquency: a test of the strength model of
self-control. J Youth Adolesc. 2015 Feb;44(2):465-77.
Mercer PW, Merritt SL, Cowell JM. Differences in reported
sleep need among adolescents. J Adolesc Health. 1998
Nov;23(5):259-63.
Michels N, Clays E, De Buyzere M, Vanaelst B, De Henauw
S, Sioen I. Children's sleep and autonomic function: low
sleep quality has an impact on heart rate variability. Sleep.
2013 Dec 1;36(12):1939-46.
Molfese DL, Ivanenko A, Key AF, Roman A, Molfese VJ,
O'Brien LM, Gozal D, Kota S, Hudac CM. A one-hour
sleep restriction impacts brain processing in young
children across tasks: evidence from event-related
potentials. Dev Neuropsychol. 2013;38(5):317-36.
Monasta L, Batty GD, Cattaneo A, Lutje V, Ronfani L, Van
Lenthe FJ, Brug J. Early-life determinants of overweight
and obesity: a review of systematic reviews. Obes Rev.
2010 Oct;11(10):695-708.
Montgomery-Downs HE, Gozal D. Sleep habits and risk
factors for sleep-disordered breathing in infants and young
toddlers in Louisville, Kentucky. Sleep Med. 2006
Apr;7(3):211-9.
Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C,
Redline S. Correlates of adolescent sleep time and
variability in sleep time: the role of individual and health
related characteristics. Sleep Med. 2011 Mar;12(3):239-
45.
Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C,
Ancoli-Israel S, Redline S. Relationships among
sleepiness, sleep time, and psychological functioning in
adolescents. J Pediatr Psychol. 2009 Nov-
Dec;34(10):1175-83.
Morley BC, Scully ML, Niven PH, Okely AD, Baur LA, Pratt
IS, Wakefield MA; NaSSDA Study Team. What factors are
associated with excess body weight in Australian
secondary school students? Med J Aust. 2012 Feb
20;196(3):189-92.
Moseley L, Gradisar M. Evaluation of a school-based
intervention for adolescent sleep problems. Sleep. 2009
Mar;32(3):334-41.
Must A, Parisi SM. Sedentary behavior and sleep:
paradoxical effects in association with childhood obesity.
Int J Obes (Lond). 2009 Apr;33 Suppl 1:S82-6.
Natal CL, Lourenço TJ, Silva LA, Boscolo RA, Silva A, Tufik
S, Mello MT. Gender differences in the sleep habits of 11-
13 year olds. Rev Bras Psiquiatr. 2009 Dec;31(4):358-61.
Ng EP, Ng DK, Chan CH. Sleep duration, wake/sleep
symptoms, and academic performance in Hong Kong
Secondary School Children. Sleep Breath. 2009
Nov;13(4):357-67.
Nixon GM, Thompson JM, Han DY, Becroft DM, Clark PM,
Robinson E, Waldie KE, Wild CJ, Black PN, Mitchell EA.
Short sleep duration in middle childhood: risk factors and
consequences. Sleep. 2008 Jan;31(1):71-8.
Noland H, Price JH, Dake J, Telljohann SK. Adolescents'
sleep behaviors and perceptions of sleep. J Sch Health.
2009 May;79(5):224-30.
O'Brien EM, Mindell JA. Sleep and risk-taking behavior in
adolescents. Behav Sleep Med. 2005;3(3):113-33.
O'Dea JA, Dibley MJ, Rankin NM. Low sleep and low
socioeconomic status predict high body mass index: a 4-
year longitudinal study of Australian schoolchildren.
Pediatr Obes. 2012 Aug;7(4):295-303.
Ohida T, Osaki Y, Doi Y, Tanihata T, Minowa M, Suzuki K,
Wada K, Suzuki K, Kaneita Y. An epidemiologic study of
self-reported sleep problems among Japanese
adolescents. Sleep. 2004 Aug 1;27(5):978-85.
Olds T, Maher C, Blunden S, Matricciani L. Normative data
on the sleep habits of Australian children and adolescents.
Sleep. 2010 Oct;33(10):1381-8.
Olds T, Blunden S, Petkov J, Forchino F. The relationships
between sex, age, geography and time in bed in
adolescents: a meta-analysis of data from 23 countries.
Sleep Med Rev. 2010 Dec;14(6):371-8.
Olds TS, Maher CA, Matricciani L. Sleep duration or
bedtime? Exploring the relationship between sleep habits
and weight status and activity patterns. Sleep. 2011 Oct
1;34(10):1299-307.
Ortega FB, Ruiz JR, Labayen I, Kwak L, Harro J, Oja L,
Veidebaum T, Sjöström M. Sleep duration and activity
levels in Estonian and Swedish children and adolescents.
Eur J Appl Physiol. 2011 Oct;111(10):2615-23.
Ortega FB, Chillón P, Ruiz JR, Delgado M, Albers U,
Alvarez-Granda JL, Marcos A, Moreno LA, Castillo MJ.
Sleep patterns in Spanish adolescents: associations with
TV watching and leisure-time physical activity. Eur J Appl
Physiol. 2010 Oct;110(3):563-73.
Owens J. Classification and epidemiology of childhood sleep
disorders. Prim Care. 2008 Sep;35(3):533-46, vii.
Owens J, Maxim R, McGuinn M, Nobile C, Msall M, Alario A.
Television-viewing habits and sleep disturbance in school
children. Pediatrics. 1999 Sep;104(3):e27.
Owens JA, Belon K, Moss P. Impact of delaying school start
time on adolescent sleep, mood, and behavior. Arch
Pediatr Adolesc Med. 2010 Jul;164(7):608-14.
Owens JA, Fernando S, Mc Guinn M. Sleep disturbance and
injury risk in young children. Behav Sleep Med.
2005;3(1):18-31.
Paavonen EJ, Räikkönen K, Pesonen AK, Lahti J, Komsi N,
Heinonen K, Järvenpää AL, Strandberg T, Kajantie E,
Porkka-Heiskanen T. Sleep quality and cognitive
performance in 8-year-old children. Sleep Med. 2010
Apr;11(4):386-92.
Paavonen EJ, Vehkalahti K, Vanhala R, von Wendt L,
Nieminen-von Wendt T, Aronen ET. Sleep in children with
Asperger syndrome. J Autism Dev Disord. 2008
Jan;38(1):41-51.
Paavonen EJ, Nieminen-von Wendt T, Vanhala R, Aronen
ET, von Wendt L. Effectiveness of melatonin in the
treatment of sleep disturbances in children with Asperger
disorder. J Child Adolesc Psychopharmacol. 2003
Spring;13(1):83-95.
Paciência I, Barros H, Araújo J, Ramos E. Association
between sleep duration and blood pressure in
adolescents. Hypertens Res. 2013 Aug;36(8):747-52.
Paksarian D, Rudolph KE, He JP, Merikangas KR. School
Start Time and Adolescent Sleep Patterns: Results From
the U.S. National Comorbidity Survey--Adolescent
Supplement. Am J Public Health. 2015 Jul;105(7):1351-7.
Paraskakis E, Ntouros T, Ntokos M, Siavana O, Bitsori M,
Galanakis E. Siesta and sleep patterns in a sample of
adolescents in Greece. Pediatr Int. 2008 Oct;50(5):690-3.
Park JH, Yoo JH, Kim SH. Associations between non-
restorative sleep, short sleep duration and suicidality:
findings from a representative sample of Korean
adolescents. Psychiatry Clin Neurosci. 2013 Jan;67(1):28-
34.
Park S. The association between short sleep duration and
body mass index among South Korean children and
adolescents. J Sch Nurs. 2013 Apr;29(2):142-50.
Park YM, Matsumoto K, Seo YJ, Shinkoda H. Sleep and
chronotype for children in Japan. Percept Mot Skills. 1999
Jun;88(3 Pt 2):1315-29.
Pasch KE, Latimer LA, Cance JD, Moe SG, Lytle LA.
Longitudinal bi-directional relationships between sleep and
youth substance use. J Youth Adolesc. 2012
Sep;41(9):1184-96.
Pasch KE, Laska MN, Lytle LA, Moe SG. Adolescent sleep,
risk behaviors, and depressive symptoms: are they linked?
Am J Health Behav. 2010 Mar-Apr;34(2):237-48.
Peach H, Gaultney JF, Reeve CL. Sleep characteristics,
body mass index, and risk for hypertension in young
adolescents. J Youth Adolesc. 2015 Feb;44(2):271-84.
Perez-Chada D, Perez-Lloret S, Videla AJ, Cardinali D,
Bergna MA, Fernández-Acquier M, Larrateguy L, Zabert
GE, Drake C. Sleep disordered breathing and daytime
sleepiness are associated with poor academic
performance in teenagers. A study using the Pediatric
Daytime Sleepiness Scale (PDSS). Sleep. 2007
Dec;30(12):1698-703.
Perez-Lloret S, Videla AJ, Richaudeau A, Vigo D, Rossi M,
Cardinali DP, Perez-Chada D. A multi-step pathway
connecting short sleep duration to daytime somnolence,
reduced attention, and poor academic performance: an
exploratory cross-sectional study in teenagers. J Clin
Sleep Med. 2013 May 15;9(5):469-73.
Pesonen AK, Martikainen S, Kajantie E, Heinonen K,
Wehkalampi K, Lahti J, Strandberg T, Räikkönen K. The
associations between adolescent sleep, diurnal cortisol
patterns and cortisol reactivity to dexamethasone
suppression test. Psychoneuroendocrinology. 2014
Nov;49:150-60.
Pesonen AK, Sjöstén NM, Matthews KA, Heinonen K,
Martikainen S, Kajantie E, Tammelin T, Eriksson JG,
Strandberg T, Räikkönen K. Temporal associations
between daytime physical activity and sleep in children.
PLoS One. 2011;6(8):e22958.
Randler C. Differences in sleep and circadian preference
between Eastern and Western German adolescents.
Chronobiol Int. 2008 Jul;25(4):565-75.
Reid A, Maldonado CC, Baker FC. Sleep behavior of South
African adolescents. Sleep. 2002 Jun 15;25(4):423-7.
Rey-López JP, de Carvalho HB, de Moraes AC, Ruiz JR,
Sjöström M, Marcos A, Polito A, Gottrand F, Manios Y,
Kafatos A, Molnar D, Widhalm K, De Henauw S, Moreno
LA; HELENA study. Sleep time and cardiovascular risk
factors in adolescents: the HELENA (Healthy Lifestyle in
Europe by Nutrition in Adolescence) study. Sleep Med.
2014 Jan;15(1):104-10.
Roberts RE, Duong HT. The prospective association
between sleep deprivation and depression among
adolescents. Sleep. 2014 Feb 1;37(2):239-44.
Russo PM, Bruni O, Lucidi F, Ferri R, Violani C. Sleep habits
and circadian preference in Italian children and
adolescents. J Sleep Res. 2007 Jun;16(2):163-9.
Räikkönen K, Matthews KA, Pesonen AK, Pyhälä R,
Paavonen EJ, Feldt K, Jones A, Phillips DI, Seckl JR,
Heinonen K, Lahti J, Komsi N, Järvenpää AL, Eriksson
JG, Strandberg TE, Kajantie E. Poor sleep and altered
hypothalamic-pituitary-adrenocortical and sympatho-
adrenal-medullary system activity in children. J Clin
Endocrinol Metab. 2010 May;95(5):2254-61.
Sadeh A, Gruber R, Raviv A. The effects of sleep restriction
and extension on school-age children: what a difference
an hour makes. Child Dev. 2003 Mar-Apr;74(2):444-55.
Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral
functioning, and behavior problems in school-age children.
Child Dev. 2002 Mar-Apr;73(2):405-17.
Schreck KA, Mulick JA, Smith AF. Sleep problems as
possible predictors of intensified symptoms of autism. Res
Dev Disabil. 2004 Jan-Feb;25(1):57-66.
Shan XY, Xi B, Cheng H, Hou DQ, Wang Y, Mi J.
Prevalence and behavioral risk factors of overweight and
obesity among children aged 2-18 in Beijing, China. Int J
Pediatr Obes. 2010 Oct;5(5):383-9.
Shochat T, Cohen-Zion M, Tzischinsky O. Functional
consequences of inadequate sleep in adolescents: a
systematic review. Sleep Med Rev. 2014 Feb;18(1):75-87.
Shochat T, Flint-Bretler O, Tzischinsky O. Sleep patterns,
electronic media exposure and daytime sleep-related
behaviours among Israeli adolescents. Acta Paediatr.
2010 Sep;99(9):1396-400.
Short MA, Gradisar M, Lack LC, Wright HR, Dohnt H. The
sleep patterns and well-being of Australian adolescents. J
Adolesc. 2013 Feb;36(1):103-10.
Short MA, Gradisar M, Lack LC, Wright HR. The impact of
sleep on adolescent depressed mood, alertness and
academic performance. J Adolesc. 2013 Dec;36(6):1025-
33.
Shur-Fen Gau S. Prevalence of sleep problems and their
association with inattention/hyperactivity among children
aged 6-15 in Taiwan. J Sleep Res. 2006 Dec;15(4):403-
14. Erratum in: J Sleep Res. 2010 Jun;19(2):379. Shur-
Fen, Gau Susan [corrected to Shur-Fen Gau, Susan].
Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen
L, Ystrom E, Hysing M. Later emotional and behavioral
problems associated with sleep problems in toddlers: a
longitudinal study. JAMA Pediatr. 2015 Jun;169(6):575-82.
Sivertsen B, Harvey AG, Lundervold AJ, Hysing M. Sleep
problems and depression in adolescence: results from a
large population-based study of Norwegian adolescents
aged 16-18 years. Eur Child Adolesc Psychiatry. 2014
Aug;23(8):681-9.
Skidmore PM, Howe AS, Polak MA, Wong JE, Lubransky A,
Williams SM, Black KE. Sleep duration and adiposity in
older adolescents from Otago, New Zealand: relationships
differ between boys and girls and are independent of food
choice. Nutr J. 2013 Sep 14;12:128.
Souders MC, Mason TB, Valladares O, Bucan M, Levy SE,
Mandell DS, Weaver TE, Pinto-Martin J. Sleep behaviors
and sleep quality in children with autism spectrum
disorders. Sleep. 2009 Dec;32(12):1566-78.
Spilsbury JC, Storfer-Isser A, Drotar D, Rosen CL, Kirchner
HL, Redline S. Effects of the home environment on
school-aged children's sleep. Sleep. 2005
Nov;28(11):1419-27.
Spilsbury JC, Storfer-Isser A, Drotar D, Rosen CL, Kirchner
LH, Benham H, Redline S. Sleep behavior in an urban US
sample of school-aged children. Arch Pediatr Adolesc
Med. 2004 Oct;158(10):988-94.
Spruyt K, Aitken RJ, So K, Charlton M, Adamson TM, Horne
RS. Relationship between sleep/wake patterns,
temperament and overall development in term infants over
the first year of life. Early Hum Dev. 2008 May;84(5):289-
96.
Stea TH, Knutsen T, Torstveit MK. Association between
short time in bed, health-risk behaviors and poor academic
achievement among Norwegian adolescents. Sleep Med.
2014 Jun;15(6):666-71.
Steele RM, van Sluijs EM, Cassidy A, Griffin SJ, Ekelund U.
Targeting sedentary time or moderate- and vigorous-
intensity activity: independent relations with adiposity in a
population-based sample of 10-y-old British children. Am J
Clin Nutr. 2009 Nov;90(5):1185-92.
Steenari MR, Vuontela V, Paavonen EJ, Carlson S, Fjallberg
M, Aronen E. Working memory and sleep in 6- to 13-year-
old schoolchildren. J Am Acad Child Adolesc Psychiatry.
2003 Jan;42(1):85-92.
Sugimori H, Yoshida K, Izuno T, Miyakawa M, Suka M,
Sekine M, Yamagami T, Kagamimori S. Analysis of factors
that influence body mass index from ages 3 to 6 years: A
study based on the Toyama cohort study. Pediatr Int. 2004
Jun;46(3):302-10.
Sun Y, Sekine M, Kagamimori S. Lifestyle and overweight
among Japanese adolescents: the Toyama Birth Cohort
Study. J Epidemiol. 2009;19(6):303-10.
Suzuki H, Kaneita Y, Osaki Y, Minowa M, Kanda H, Suzuki
K, Wada K, Hayashi K, Tanihata T, Ohida T. Clarification
of the factor structure of the 12-item General Health
Questionnaire among Japanese adolescents and
associated sleep status. Psychiatry Res. 2011 Jun
30;188(1):138-46.
Takemura T, Funaki K, Kanbayashi T, Kawamoto K, Tsutsui
K, Saito Y, Aizawa R, Inomata S, Shimizu T. Sleep habits
of students attending elementary schools, and junior and
senior high schools in Akita prefecture. Psychiatry Clin
Neurosci. 2002 Jun;56(3):241-2.
Tatone-Tokuda F, Dubois L, Ramsay T, Girard M, Touchette
E, Petit D, Montplaisir JY. Sex differences in the
association between sleep duration, diet and body mass
index: a birth cohort study. J Sleep Res. 2012
Aug;21(4):448-60.
Taylor DJ, Jenni OG, Acebo C, Carskadon MA. Sleep
tendency during extended wakefulness: insights into
adolescent sleep regulation and behavior. J Sleep Res.
2005 Sep;14(3):239-44.
Taylor RW, Williams SM, Farmer VL, Taylor BJ. The stability
of sleep patterns in children 3 to 7 years of age. J Pediatr.
2015 Mar;166(3):697-702.e1.
Teixeira LR, Fischer FM, de Andrade MM, Louzada FM,
Nagai R. Sleep patterns of day-working, evening high-
schooled adolescents of São Paulo, Brazil. Chronobiol
Int. 2004 Mar;21(2):239-52.
Thorpe K, Staton S, Sawyer E, Pattinson C, Haden C, Smith
S. Napping, development and health from 0 to 5 years: a
systematic review. Arch Dis Child. 2015 Jul;100(7):615-22.
Touchette E, Côté SM, Petit D, Liu X, Boivin M, Falissard B,
Tremblay RE, Montplaisir JY. Short nighttime sleep-
duration and hyperactivity trajectories in early childhood.
Pediatrics. 2009 Nov;124(5):e985-93.
Unalan D, Ozturk A, Ismailogullari S, Akgul N, Aksu M. The
effect of sleep duration and quality on academical success
of the elementary school children in Kayseri Turkey. J Pak
Med Assoc. 2013 May;63(5):576-80.
van der Vinne V, Zerbini G, Siersema A, Pieper A, Merrow
M, Hut RA, Roenneberg T, Kantermann T. Timing of
examinations affects school performance differently in
early and late chronotypes. J Biol Rhythms. 2015
Feb;30(1):53-60.
Vazsonyi AT, Harris C, Terveer AM, Pagava K, Phagava H,
Michaud PA. Parallel mediation effects by sleep on the
parental warmth-problem behavior links: evidence from
national probability samples of Georgian and Swiss
adolescents. J Youth Adolesc. 2015 Feb;44(2):331-45.
Verrillo E, Bizzarri C, Cappa M, Bruni O, Pavone M, Ferri R,
Cutrera R. Sleep characteristics in children with growth
hormone deficiency. Neuroendocrinology. 2011;94(1):66-
74.
Voderholzer U, Piosczyk H, Holz J, Landmann N, Feige B,
Loessl B, Kopasz M, Doerr JP, Riemann D, Nissen C.
Sleep restriction over several days does not affect long-
term recall of declarative and procedural memories in
adolescents. Sleep Med. 2011 Feb;12(2):170-8.
Vriend JL, Davidson FD, Corkum PV, Rusak B, Chambers
CT, McLaughlin EN. Manipulating sleep duration alters
emotional functioning and cognitive performance in
children. J Pediatr Psychol. 2013 Nov;38(10):1058-69.
Waldie KE, Thompson JM, Mia Y, Murphy R, Wall C,
Mitchell EA. Risk factors for migraine and tension-type
headache in 11 year old children. J Headache Pain. 2014
Sep 10;15:60.
Wang H, Sekine M, Chen X, Yamagami T, Kagamimori S.
Lifestyle at 3 years of age and quality of life (QOL) in first-
year junior high school students in Japan: results of the
Toyama Birth Cohort Study. Qual Life Res. 2008
Mar;17(2):257-65.
Weiss A, Xu F, Storfer-Isser A, Thomas A, Ievers-Landis CE,
Redline S. The association of sleep duration with
adolescents' fat and carbohydrate consumption. Sleep.
2010 Sep;33(9):1201-9.
Weissbluth M, Davis AT, Poncher J. Night waking in 4- to 8-
month-old infants. J Pediatr. 1984 Mar;104(3):477-80.
Weissbluth M, Brouillete RT, Liu K, Hunt CE. Sleep apnea,
sleep duration, and infant temperament. J Pediatr. 1982
Aug;101(2):307-10.
Weissbluth M. Sleep duration and infant temperament. J
Pediatr. 1981 Nov;99(5):817-9.
Wells JC, Hallal PC, Reichert FF, Menezes AM, Araújo CL,
Victora CG. Sleep patterns and television viewing in
relation to obesity and blood pressure: evidence from an
adolescent Brazilian birth cohort. Int J Obes (Lond). 2008
Jul;32(7):1042-9.
Westerlund L, Ray C, Roos E. Associations between
sleeping habits and food consumption patterns among 10-
11-year-old children in Finland. Br J Nutr. 2009
Nov;102(10):1531-7.
Winsler A, Deutsch A, Vorona RD, Payne PA, Szklo-Coxe
M. Sleepless in Fairfax: the difference one more hour of
sleep can make for teen hopelessness, suicidal ideation,
and substance use. J Youth Adolesc. 2015 Feb;44(2):362-
78.
Yang CK, Kim JK, Patel SR, Lee JH. Age-related changes in
sleep/wake patterns among Korean teenagers. Pediatrics.
2005 Jan;115(1 Suppl):250-6.
Yen CF, King BH, Tang TC. The association between short
and long nocturnal sleep durations and risky behaviours
and the moderating factors in Taiwanese adolescents.
Psychiatry Res. 2010 Aug 30;179(1):69-74.
Yip T. The effects of ethnic/racial discrimination and sleep
quality on depressive symptoms and self-esteem
trajectories among diverse adolescents. J Youth Adolesc.
2015 Feb;44(2):419-30.
Yokomaku A, Misao K, Omoto F, Yamagishi R, Tanaka K,
Takada K, Kohyama J. A study of the association between
sleep habits and problematic behaviors in preschool
children. Chronobiol Int. 2008 Jul;25(4):549-64.
General Health
Amschler DH, McKenzie JF. Elementary students' sleep
habits and teacher observations of sleep-related
problems. J Sch Health. 2005 Feb;75(2):50-6.
Arman AR, Ay P, Fis NP, Ersu R, Topuzoglu A, Isik U,
Berkem M. Association of sleep duration with socio-
economic status and behavioural problems among
schoolchildren. Acta Paediatr. 2011 Mar;100(3):420-4.
Bertelle V, Sevestre A, Laou-Hap K, Nagahapitiye MC, Sizun
J. Sleep in the neonatal intensive care unit. J Perinat
Neonatal Nurs. 2007 Apr-Jun;21(2):140-8; quiz 149-50.
Review.
Bertelle V, Mabin D, Adrien J, Sizun J. Sleep of preterm
neonates under developmental care or regular
environmental conditions. Early Hum Dev. 2005
Jul;81(7):595-600.
Byars KC, Yolton K, Rausch J, Lanphear B, Beebe DW.
Prevalence, patterns, and persistence of sleep problems
in the first 3 years of life. Pediatrics. 2012
Feb;129(2):e276-84.
Chugh IM, Khanna P, Shah A. Nocturnal symptoms and
sleep disturbances in clinically stable asthmatic children.
Asian Pac J Allergy Immunol. 2006 Jun-Sep;24(2-3):135-
42.
Daniel LC, Boergers J, Kopel SJ, Koinis-Mitchell D. Missed
sleep and asthma morbidity in urban children. Ann Allergy
Asthma Immunol. 2012 Jul;109(1):41-6.
El-Sheikh M, Buckhalt JA, Keller PS, Granger DA. Children's
objective and subjective sleep disruptions: links with
afternoon cortisol levels. Health Psychol. 2008
Jan;27(1):26-33.
Ertan P, Yilmaz O, Caglayan M, Sogut A, Aslan S, Yuksel H.
Relationship of sleep quality and quality of life in children
with monosymptomatic enuresis. Child Care Health Dev.
2009 Jul;35(4):469-74.
Gau SF. Neuroticism and sleep-related problems in
adolescence. Sleep. 2000 Jun 15;23(4):495-502.
Gerber L. Sleep deprivation in children: a growing public
health concern. Nursing. 2014 Apr;44(4):50-4. No abstract
available.
Hiscock H, Sciberras E, Mensah F, Gerner B, Efron D,
Khano S, Oberklaid F. Impact of a behavioural sleep
intervention on symptoms and sleep in children with
attention deficit hyperactivity disorder, and parental mental
health: randomised controlled trial. BMJ. 2015 Jan
20;350:h68.
Kostyun RO, Milewski MD, Hafeez I. Sleep disturbance and
neurocognitive function during the recovery from a sport-
related concussion in adolescents. Am J Sports Med.
2015 Mar;43(3):633-40.
Lam LT, Yang L. Short duration of sleep and unintentional
injuries among adolescents in China. Am J Epidemiol.
2007 Nov 1;166(9):1053-8.
Li Y, Jin H, Owens JA, Hu C. The association between sleep
and injury among school-aged children in rural China: a
case-control study. Sleep Med. 2008 Jan;9(2):142-8.
Lin WH, Yi CC. Unhealthy sleep practices, conduct
problems, and daytime functioning during adolescence. J
Youth Adolesc. 2015 Feb;44(2):431-46.
Magee CA, Lee JK, Vella SA. Bidirectional relationships
between sleep duration and screen time in early
childhood. JAMA Pediatr. 2014 May;168(5):465-70.
Magee CA, Gordon R, Caputi P. Distinct developmental
trends in sleep duration during early childhood. Pediatrics.
2014 Jun;133(6):e1561-7.
Matricciani L, Blunden S, Rigney G, Williams MT, Olds TS.
Children's sleep needs: is there sufficient evidence to
recommend optimal sleep for children? Sleep. 2013 Apr
1;36(4):527-34.
Matthews KA, Hall M, Dahl RE. Sleep in healthy black and
white adolescents. Pediatrics. 2014 May;133(5):e1189-96.
McHale SM, Kim JY, Kan M, Updegraff KA. Sleep in
Mexican-American adolescents: social ecological and
well-being correlates. J Youth Adolesc. 2011
Jun;40(6):666-79.
Milewski MD, Skaggs DL, Bishop GA, Pace JL, Ibrahim DA,
Wren TA, Barzdukas A. Chronic lack of sleep is
associated with increased sports injuries in adolescent
athletes. J Pediatr Orthop. 2014 Mar;34(2):129-33.
Olds T, Blunden S, Petkov J, Forchino F. The relationships
between sex, age, geography and time in bed in
adolescents: a meta-analysis of data from 23 countries.
Sleep Med Rev. 2010 Dec;14(6):371-8.
Owens JA, Fernando S, Mc Guinn M. Sleep disturbance and
injury risk in young children. Behav Sleep Med.
2005;3(1):18-31.
Paavonen EJ, Nieminen-von Wendt T, Vanhala R, Aronen
ET, von Wendt L. Effectiveness of melatonin in the
treatment of sleep disturbances in children with Asperger
disorder. J Child Adolesc Psychopharmacol. 2003
Spring;13(1):83-95.
Park YM, Matsumoto K, Seo YJ, Shinkoda H. Sleep and
chronotype for children in Japan. Percept Mot Skills. 1999
Jun;88(3 Pt 2):1315-29.
Scott N, Blair PS, Emond AM, Fleming PJ, Humphreys JS,
Henderson J, Gringras P. Sleep patterns in children with
ADHD: a population-based cohort study from birth to
11 years. J Sleep Res. 2013 Apr;22(2):121-8.
Segura-Jiménez V, Carbonell-Baeza A, Keating XD, Ruiz
JR, Castro-Piñero J. Association of sleep patterns with
psychological positive health and health complaints in
children and adolescents. Qual Life Res. 2015
Apr;24(4):885-95.
Serra-Negra JM, Paiva SM, Fulgêncio LB, Chavez BA, Lage
CF, Pordeus IA. Environmental factors, sleep duration,
and sleep bruxism in Brazilian schoolchildren: a case-
control study. Sleep Med. 2014 Feb;15(2):236-9.
Shi Z, Taylor AW, Gill TK, Tuckerman J, Adams R, Martin J.
Short sleep duration and obesity among Australian
children. BMC Public Health. 2010 Oct 15;10:609.
Short MA, Gradisar M, Lack LC, Wright HR, Dohnt H. The
sleep patterns and well-being of Australian adolescents. J
Adolesc. 2013 Feb;36(1):103-10.
Smaldone A, Honig JC, Byrne MW. Sleepless in America:
inadequate sleep and relationships to health and well-
being of our nation's children. Pediatrics. 2007 Feb;119
Suppl 1:S29-37.
Spruyt K, Alaribe CU, Nwabara OU. To sleep or not to sleep:
a repeated daily challenge for African American children.
CNS Neurosci Ther. 2015 Jan;21(1):23-31.
Stallones L, Beseler C, Chen P. Sleep patterns and risk of
injury among adolescent farm residents. Am J Prev Med.
2006 Apr;30(4):300-4.
Valent F, Brusaferro S, Barbone F. A case-crossover study
of sleep and childhood injury. Pediatrics. 2001
Feb;107(2):E23.
van der Vinne V, Zerbini G, Siersema A, Pieper A, Merrow
M, Hut RA, Roenneberg T, Kantermann T. Timing of
examinations affects school performance differently in
early and late chronotypes. J Biol Rhythms. 2015
Feb;30(1):53-60.
Vazsonyi AT, Harris C, Terveer AM, Pagava K, Phagava H,
Michaud PA. Parallel mediation effects by sleep on the
parental warmth-problem behavior links: evidence from
national probability samples of Georgian and Swiss
adolescents. J Youth Adolesc. 2015 Feb;44(2):331-45.
Wang H, Sekine M, Chen X, Yamagami T, Kagamimori S.
Lifestyle at 3 years of age and quality of life (QOL) in first-
year junior high school students in Japan: results of the
Toyama Birth Cohort Study. Qual Life Res. 2008
Mar;17(2):257-65.
Willoughby MT, Angold A, Egger HL. Parent-reported
attention-deficit/hyperactivity disorder symptomatology
and sleep problems in a preschool-age pediatric clinic
sample. J Am Acad Child Adolesc Psychiatry. 2008
Sep;47(9):1086-94.
Human Performance
Abe T, Hagihara A, Nobutomo K. Sleep patterns and
impulse control among Japanese junior high school
students. J Adolesc. 2010 Oct;33(5):633-41.
Amschler DH, McKenzie JF. Elementary students' sleep
habits and teacher observations of sleep-related
problems. J Sch Health. 2005 Feb;75(2):50-6.
Anderson B, Storfer-Isser A, Taylor HG, Rosen CL, Redline
S. Associations of executive function with sleepiness and
sleep duration in adolescents. Pediatrics. 2009
Apr;123(4):e701-7.
Andrade MM, Benedito-Silva AA, Domenice S, Arnhold IJ,
Menna-Barreto L. Sleep characteristics of adolescents: a
longitudinal study. J Adolesc Health. 1993 Jul;14(5):401-6.
Arakawa M, Taira K, Tanaka H, Yamakawa K, Toguchi H,
Kadekaru H, Yamamoto Y, Uezu E, Shirakawa S. A
survey of junior high school students' sleep habit and
lifestyle in Okinawa. Psychiatry Clin Neurosci. 2001
Jun;55(3):211-2.
Astill RG, Van der Heijden KB, Van Ijzendoorn MH, Van
Someren EJ. Sleep, cognition, and behavioral problems in
school-age children: a century of research meta-analyzed.
Psychol Bull. 2012 Nov;138(6):1109-38.
Beebe DW, Ris MD, Kramer ME, Long E, Amin R. The
association between sleep disordered breathing,
academic grades, and cognitive and behavioral
functioning among overweight subjects during middle to
late childhood. Sleep. 2010 Nov;33(11):1447-56.
Beebe DW, Rose D, Amin R. Attention, learning, and arousal
of experimentally sleep-restricted adolescents in a
simulated classroom. J Adolesc Health. 2010
Nov;47(5):523-5.
Bell JF, Zimmerman FJ. Shortened nighttime sleep duration
in early life and subsequent childhood obesity. Arch
Pediatr Adolesc Med. 2010 Sep;164(9):840-5. Erratum in:
Arch Pediatr Adolesc Med. 2010 Nov;164(11):1070.
Blunden SL, Beebe DW. The contribution of intermittent
hypoxia, sleep debt and sleep disruption to daytime
performance deficits in children: consideration of
respiratory and non-respiratory sleep disorders. Sleep
Med Rev. 2006 Apr;10(2):109-18.
Boto LR, Crispim JN, de Melo IS, Juvandes C, Rodrigues T,
Azeredo P, Ferreira R. Sleep deprivation and accidental
fall risk in children. Sleep Med. 2012 Jan;13(1):88-95.
Buckhalt JA, El-Sheikh M, Keller P. Children's sleep and
cognitive functioning: race and socioeconomic status as
moderators of effects. Child Dev. 2007 Jan-Feb;78(1):213-
31.
Carskadon MA. Sleep's effects on cognition and learning in
adolescence. Prog Brain Res. 2011;190:137-43.
Chung KF, Cheung MM. Sleep-wake patterns and sleep
disturbance among Hong Kong Chinese adolescents.
Sleep. 2008 Feb;31(2):185-94.
Cortese S, Konofal E, Yateman N, Mouren MC, Lecendreux
M. Sleep and alertness in children with attention-
deficit/hyperactivity disorder: a systematic review of the
literature. Sleep. 2006 Apr;29(4):504-11. Review.
Countryman AJ, Saab PG, Llabre MM, Penedo FJ, McCalla
JR, Schneiderman N. Cardiometabolic risk in adolescents:
associations with physical activity, fitness, and sleep. Ann
Behav Med. 2013 Feb;45(1):121-31.
Dahl RE. Biological, developmental, and neurobehavioral
factors relevant to adolescent driving risks. Am J Prev
Med. 2008 Sep;35(3 Suppl):S278-84.
Dahl RE, Ryan ND, Matty MK, Birmaher B, al-Shabbout M,
Williamson DE, Kupfer DJ. Sleep onset abnormalities in
depressed adolescents. Biol Psychiatry. 1996 Mar
15;39(6):400-10.
Davis AL, Avis KT, Schwebel DC. The effects of acute sleep
restriction on adolescents' pedestrian safety in a virtual
environment. J Adolesc Health. 2013 Dec;53(6):785-90.
El-Sheikh M, Buckhalt JA, Mark Cummings E, Keller P.
Sleep disruptions and emotional insecurity are pathways
of risk for children. J Child Psychol Psychiatry. 2007
Jan;48(1):88-96.
Escribano C, Díaz-Morales JF. Daily fluctuations in attention
at school considering starting time and chronotype: an
exploratory study. Chronobiol Int. 2014 Jul;31(6):761-9.
Fallone G, Acebo C, Seifer R, Carskadon MA. Experimental
restriction of sleep opportunity in children: effects on
teacher ratings. Sleep. 2005 Dec;28(12):1561-7.
Franco P, Seret N, Van Hees JN, Lanquart JP Jr,
Groswasser J, Kahn A. Cardiac changes during sleep in
sleep-deprived infants. Sleep. 2003 Nov 1;26(7):845-8.
Fukuda K, Sakashita Y. Sleeping pattern of kindergartners
and nursery school children: function of daytime nap.
Percept Mot Skills. 2002 Feb;94(1):219-28.
Garmy P, Nyberg P, Jakobsson U. Sleep and television and
computer habits of Swedish school-age children. J Sch
Nurs. 2012 Dec;28(6):469-76.
Gau SF. Neuroticism and sleep-related problems in
adolescence. Sleep. 2000 Jun 15;23(4):495-502.
Gau SS, Shang CY, Merikangas KR, Chiu YN, Soong WT,
Cheng AT. Association between morningness-
eveningness and behavioral/emotional problems among
adolescents. J Biol Rhythms. 2007 Jun;22(3):268-74.
Geiger A, Achermann P, Jenni OG. Association between
sleep duration and intelligence scores in healthy children.
Dev Psychol. 2010 Jul;46(4):949-54.
Gibbs S, Wiltshire E, Elder D. Nocturnal sleep measured by
actigraphy in children with Prader-Willi syndrome. J
Pediatr. 2013 Apr;162(4):765-9.
Gibson ES, Powles AC, Thabane L, O'Brien S, Molnar DS,
Trajanovic N, Ogilvie R, Shapiro C, Yan M, Chilcott-
Tanser L. Sleepiness" is serious in adolescence: two
surveys of 3235 Canadian students." BMC Public Health.
2006 May 2;6:116.
Greenfeld M, Constantini S, Tauman R, Sivan Y. Sleep
disturbances in children recovered from central nervous
system neoplasms. J Pediatr. 2011 Aug;159(2):268-72.e1.
Gruber R, Cassoff J, Frenette S, Wiebe S, Carrier J. Impact
of sleep extension and restriction on children's emotional
lability and impulsivity. Pediatrics. 2012 Nov;130(5):e1155-
61.
Gruber R, Wiebe S, Montecalvo L, Brunetti B, Amsel R,
Carrier J. Impact of sleep restriction on neurobehavioral
functioning of children with attention deficit hyperactivity
disorder. Sleep. 2011 Mar 1;34(3):315-23.
Gruber R, Laviolette R, Deluca P, Monson E, Cornish K,
Carrier J. Short sleep duration is associated with poor
performance on IQ measures in healthy school-age
children. Sleep Med. 2010 Mar;11(3):289-94.
Guérin N, Reinberg A, Testu F, Boulenguiez S, Mechkouri
M, Touitou Y. Role of school schedule, age, and parental
socioeconomic status on sleep duration and sleepiness of
Parisian children. Chronobiol Int. 2001 Nov;18(6):1005-17.
Hansen M, Janssen I, Schiff A, Zee PC, Dubocovich ML.
The impact of school daily schedule on adolescent sleep.
Pediatrics. 2005 Jun;115(6):1555-61.
Henderson JM, France KG, Owens JL, Blampied NM.
Sleeping through the night: the consolidation of self-
regulated sleep across the first year of life. Pediatrics.
2010 Nov;126(5):e1081-7.
Hjorth MF, Chaput JP, Ritz C, Dalskov SM, Andersen R,
Astrup A, Tetens I, Michaelsen KF, Sjödin A. Fatness
predicts decreased physical activity and increased
sedentary time, but not vice versa: support from a
longitudinal study in 8- to 11-year-old children. Int J Obes
(Lond). 2014 Jul;38(7):959-65.
Holm SM, Forbes EE, Ryan ND, Phillips ML, Tarr JA, Dahl
RE. Reward-related brain function and sleep in pre/early
pubertal and mid/late pubertal adolescents. J Adolesc
Health. 2009 Oct;45(4):326-34.
Ishihara K. The effect of 2-h sleep reduction by a delayed
bedtime on daytime sleepiness in children. Psychiatry Clin
Neurosci. 1999 Apr;53(2):113-5.
Ishihara K, Miyake S. A longitudinal study of the
development of daytime sleepiness in children. Psychiatry
Clin Neurosci. 1998 Apr;52(2):178-81.
Keller PS, El-Sheikh M, Buckhalt JA. Children's attachment
to parents and their academic functioning: sleep
disruptions as moderators of effects. J Dev Behav Pediatr.
2008 Dec;29(6):441-9.
Kopasz M, Loessl B, Valerius G, Koenig E, Matthaeas N,
Hornyak M, Kloepfer C, Nissen C, Riemann D,
Voderholzer U. No persisting effect of partial sleep
curtailment on cognitive performance and declarative
memory recall in adolescents. J Sleep Res. 2010 Mar;19(1
Pt 1):71-9.
Kostyun RO, Milewski MD, Hafeez I. Sleep disturbance and
neurocognitive function during the recovery from a sport-
related concussion in adolescents. Am J Sports Med.
2015 Mar;43(3):633-40.
Lam JC, Mahone EM, Mason T, Scharf SM. The effects of
napping on cognitive function in preschoolers. J Dev
Behav Pediatr. 2011 Feb-Mar;32(2):90-7.
Lee JA, Park HS. Relation between sleep duration,
overweight, and metabolic syndrome in Korean
adolescents. Nutr Metab Cardiovasc Dis. 2014
Jan;24(1):65-71.
Leproult R, Van Cauter E. Role of sleep and sleep loss in
hormonal release and metabolism. Endocr Dev.
2010;17:11-21.
Lewandowski AS, Palermo TM, De la Motte S, Fu R.
Temporal daily associations between pain and sleep in
adolescents with chronic pain versus healthy adolescents.
Pain. 2010 Oct;151(1):220-5.
Li S, Arguelles L, Jiang F, Chen W, Jin X, Yan C, Tian Y,
Hong X, Qian C, Zhang J, Wang X, Shen X. Sleep, school
performance, and a school-based intervention among
school-aged children: a sleep series study in China. PLoS
One. 2013 Jul 10;8(7):e67928.
Lin WH, Yi CC. Unhealthy sleep practices, conduct
problems, and daytime functioning during adolescence. J
Youth Adolesc. 2015 Feb;44(2):431-46.
Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004
Nov 1;27(7):1351-8.
Mak KK, Lee SL, Ho SY, Lo WS, Lam TH. Sleep and
academic performance in Hong Kong adolescents. J Sch
Health. 2012 Nov;82(11):522-7.
Martikainen S, Pesonen AK, Feldt K, Jones A, Lahti J,
Pyhälä R, Heinonen K, Kajantie E, Eriksson J, Räikkönen
K. Poor sleep and cardiovascular function in children.
Hypertension. 2011 Jul;58(1):16-21.
Martinez-Gomez D, Eisenmann JC, Gomez-Martinez S, Hill
EE, Zapatera B, Veiga OL, Marcos A; AFINOS Study
Group. Sleep duration and emerging cardiometabolic risk
markers in adolescents. The AFINOS study. Sleep Med.
2011 Dec;12(10):997-1002.
Maski KP, Kothare SV. Sleep deprivation and
neurobehavioral functioning in children. Int J
Psychophysiol. 2013 Aug;89(2):259-64.
Matsushita M, Koyama A, Ushijima H, Mikami A, Katsumata
Y, Kikuchi Y, Ichimi N, Jono T, Fujise N, Ikeda M. Sleep
duration and its association with sleepiness and
depression in ronin-sei" preparatory school students."
Asian J Psychiatr. 2014 Jun;9:61-6.
McLaughlin Crabtree V, Beal Korhonen J, Montgomery-
Downs HE, Faye Jones V, O'Brien LM, Gozal D. Cultural
influences on the bedtime behaviors of young children.
Sleep Med. 2005 Jul;6(4):319-24.
Meijer AM. Chronic sleep reduction, functioning at school
and school achievement in preadolescents. J Sleep Res.
2008 Dec;17(4):395-405. Erratum in: J Sleep Res. 2009
Mar;18(1):144.
Mercer PW, Merritt SL, Cowell JM. Differences in reported
sleep need among adolescents. J Adolesc Health. 1998
Nov;23(5):259-63.
Mercier L, Pivik RT, Busby K. Sleep patterns in reading
disabled children. Sleep. 1993 Apr;16(3):207-15. Review.
Michels N, Clays E, De Buyzere M, Vanaelst B, De Henauw
S, Sioen I. Children's sleep and autonomic function: low
sleep quality has an impact on heart rate variability. Sleep.
2013 Dec 1;36(12):1939-46.
Molfese DL, Ivanenko A, Key AF, Roman A, Molfese VJ,
O'Brien LM, Gozal D, Kota S, Hudac CM. A one-hour
sleep restriction impacts brain processing in young
children across tasks: evidence from event-related
potentials. Dev Neuropsychol. 2013;38(5):317-36.
Ng EP, Ng DK, Chan CH. Sleep duration, wake/sleep
symptoms, and academic performance in Hong Kong
Secondary School Children. Sleep Breath. 2009
Nov;13(4):357-67.
Nugent R, Althouse A, Yaqub Y, Nugent K, Raj R. Modeling
the relation between obesity and sleep parameters in
children referred for dietary weight reduction intervention.
South Med J. 2014 Aug;107(8):473-80.
Olds T, Blunden S, Petkov J, Forchino F. The relationships
between sex, age, geography and time in bed in
adolescents: a meta-analysis of data from 23 countries.
Sleep Med Rev. 2010 Dec;14(6):371-8.
Ortega FB, Chillón P, Ruiz JR, Delgado M, Albers U,
Alvarez-Granda JL, Marcos A, Moreno LA, Castillo MJ.
Sleep patterns in Spanish adolescents: associations with
TV watching and leisure-time physical activity. Eur J Appl
Physiol. 2010 Oct;110(3):563-73.
Ortega FB, Ruiz JR, Castillo R, Chillón P, Labayen I,
Martínez-Gómez D, Redondo C, Marcos A, Moreno LA;
AVENA study group. Sleep duration and cognitive
performance in adolescence. The AVENA study. Acta
Paediatr. 2010 Mar;99(3):454-6.
Owens JA, Belon K, Moss P. Impact of delaying school start
time on adolescent sleep, mood, and behavior. Arch
Pediatr Adolesc Med. 2010 Jul;164(7):608-14.
Owens JA, Fernando S, Mc Guinn M. Sleep disturbance and
injury risk in young children. Behav Sleep Med.
2005;3(1):18-31.
Perez-Lloret S, Videla AJ, Richaudeau A, Vigo D, Rossi M,
Cardinali DP, Perez-Chada D. A multi-step pathway
connecting short sleep duration to daytime somnolence,
reduced attention, and poor academic performance: an
exploratory cross-sectional study in teenagers. J Clin
Sleep Med. 2013 May 15;9(5):469-73.
Perkinson-Gloor N, Lemola S, Grob A. Sleep duration,
positive attitude toward life, and academic achievement:
the role of daytime tiredness, behavioral persistence, and
school start times. J Adolesc. 2013 Apr;36(2):311-8.
Pesonen AK, Martikainen S, Kajantie E, Heinonen K,
Wehkalampi K, Lahti J, Strandberg T, Räikkönen K. The
associations between adolescent sleep, diurnal cortisol
patterns and cortisol reactivity to dexamethasone
suppression test. Psychoneuroendocrinology. 2014
Nov;49:150-60.
Pizza F, Contardi S, Antognini AB, Zagoraiou M, Borrotti M,
Mostacci B, Mondini S, Cirignotta F. Sleep quality and
motor vehicle crashes in adolescents. J Clin Sleep Med.
2010 Feb 15;6(1):41-5.
Reid A, Maldonado CC, Baker FC. Sleep behavior of South
African adolescents. Sleep. 2002 Jun 15;25(4):423-7.
Rey-López JP, de Carvalho HB, de Moraes AC, Ruiz JR,
Sjöström M, Marcos A, Polito A, Gottrand F, Manios Y,
Kafatos A, Molnar D, Widhalm K, De Henauw S, Moreno
LA; HELENA study. Sleep time and cardiovascular risk
factors in adolescents: the HELENA (Healthy Lifestyle in
Europe by Nutrition in Adolescence) study. Sleep Med.
2014 Jan;15(1):104-10.
Roberts RE, Roberts CR, Duong HT. Sleepless in
adolescence: prospective data on sleep deprivation,
health and functioning. J Adolesc. 2009 Oct;32(5):1045-
57.
Sadeh A, Gruber R, Raviv A. The effects of sleep restriction
and extension on school-age children: what a difference
an hour makes. Child Dev. 2003 Mar-Apr;74(2):444-55.
Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral
functioning, and behavior problems in school-age children.
Child Dev. 2002 Mar-Apr;73(2):405-17.
Sallinen BJ, Hassan F, Olszewski A, Maupin A, Hoban TF,
Chervin RD, Woolford SJ. Longer weekly sleep duration
predicts greater 3-month BMI reduction among obese
adolescents attending a clinical multidisciplinary weight
management program. Obes Facts. 2013;6(3):239-46.
Salzarulo P, Fagioli I. Sleep for development or development
for waking?--some speculations from a human
perspective. Behav Brain Res. 1995 Jul-Aug;69(1-2):23-7.
Review.
Sampei M, Murata K, Dakeishi M, Wood DC. Cardiac
autonomic hypofunction in preschool children with short
nocturnal sleep. Tohoku J Exp Med. 2006 Mar;208(3):235-
42.
Segura-Jiménez V, Carbonell-Baeza A, Keating XD, Ruiz
JR, Castro-Piñero J. Association of sleep patterns with
psychological positive health and health complaints in
children and adolescents. Qual Life Res. 2015
Apr;24(4):885-95.
Shochat T, Flint-Bretler O, Tzischinsky O. Sleep patterns,
electronic media exposure and daytime sleep-related
behaviours among Israeli adolescents. Acta Paediatr.
2010 Sep;99(9):1396-400.
Short MA, Gradisar M, Lack LC, Wright HR. The impact of
sleep on adolescent depressed mood, alertness and
academic performance. J Adolesc. 2013 Dec;36(6):1025-
33.
Spicuzza L, Sciuto C, Leonardi S, La Rosa M. Early
occurrence of obstructive sleep apnea in infants and
children with cystic fibrosis. Arch Pediatr Adolesc Med.
2012 Dec;166(12):1165-9.
Stallones L, Beseler C, Chen P. Sleep patterns and risk of
injury among adolescent farm residents. Am J Prev Med.
2006 Apr;30(4):300-4.
Steele RM, van Sluijs EM, Cassidy A, Griffin SJ, Ekelund U.
Targeting sedentary time or moderate- and vigorous-
intensity activity: independent relations with adiposity in a
population-based sample of 10-y-old British children. Am J
Clin Nutr. 2009 Nov;90(5):1185-92.
Steenari MR, Vuontela V, Paavonen EJ, Carlson S, Fjallberg
M, Aronen E. Working memory and sleep in 6- to 13-year-
old schoolchildren. J Am Acad Child Adolesc Psychiatry.
2003 Jan;42(1):85-92.
Taki Y, Hashizume H, Thyreau B, Sassa Y, Takeuchi H, Wu
K, Kotozaki Y, Nouchi R, Asano M, Asano K, Fukuda H,
Kawashima R. Sleep duration during weekdays affects
hippocampal gray matter volume in healthy children.
Neuroimage. 2012 Mar;60(1):471-5.
Teixeira LR, Fischer FM, Nagai R, Turte SL. Teen at work:
the burden of a double shift on daily activities. Chronobiol
Int. 2004;21(6):845-58.
Touchette E, Petit D, Séguin JR, Boivin M, Tremblay RE,
Montplaisir JY. Associations between sleep duration
patterns and behavioral/cognitive functioning at school
entry. Sleep. 2007 Sep;30(9):1213-9.
Unalan D, Ozturk A, Ismailogullari S, Akgul N, Aksu M. The
effect of sleep duration and quality on academical success
of the elementary school children in Kayseri Turkey. J Pak
Med Assoc. 2013 May;63(5):576-80.
Urschitz MS, Heine K, Brockmann PE, Peters T, Durst W,
Poets CF, Wilhelm B. Subjective and objective daytime
sleepiness in schoolchildren and adolescents: results of a
community-based study. Sleep Med. 2013
Oct;14(10):1005-12.
Valent F, Brusaferro S, Barbone F. A case-crossover study
of sleep and childhood injury. Pediatrics. 2001
Feb;107(2):E23.
Verrillo E, Bizzarri C, Cappa M, Bruni O, Pavone M, Ferri R,
Cutrera R. Sleep characteristics in children with growth
hormone deficiency. Neuroendocrinology. 2011;94(1):66-
74.
Voderholzer U, Piosczyk H, Holz J, Landmann N, Feige B,
Loessl B, Kopasz M, Doerr JP, Riemann D, Nissen C.
Sleep restriction over several days does not affect long-
term recall of declarative and procedural memories in
adolescents. Sleep Med. 2011 Feb;12(2):170-8.
Vriend JL, Davidson FD, Corkum PV, Rusak B, Chambers
CT, McLaughlin EN. Manipulating sleep duration alters
emotional functioning and cognitive performance in
children. J Pediatr Psychol. 2013 Nov;38(10):1058-69.
Westerlund L, Ray C, Roos E. Associations between
sleeping habits and food consumption patterns among 10-
11-year-old children in Finland. Br J Nutr. 2009
Nov;102(10):1531-7.
Zhu Y, Li AM, Au CT, Kong AP, Zhang J, Wong CK, Chan
JC, Wing YK. Association between sleep architecture and
glucose tolerance in children and adolescents. J Diabetes.
2015 Jan;7(1):10-5.
Immunologic Health
Berentzen NE, Smit HA, Bekkers MB, Brunekreef B,
Koppelman GH, De Jongste JC, Kerkhof M, Van Rossem
L, Wijga AH. Time in bed, sleep quality and associations
with cardiometabolic markers in children: the Prevention
and Incidence of Asthma and Mite Allergy birth cohort
study. J Sleep Res. 2014 Feb;23(1):3-12.
Börnhorst C, Hense S, Ahrens W, Hebestreit A, Reisch L,
Barba G, von Kries R, Bayer O; IDEFICS Consortium.
From sleep duration to childhood obesity--what are the
pathways? Eur J Pediatr. 2012 Jul;171(7):1029-38.
Chugh IM, Khanna P, Shah A. Nocturnal symptoms and
sleep disturbances in clinically stable asthmatic children.
Asian Pac J Allergy Immunol. 2006 Jun-Sep;24(2-3):135-
42.
Countryman AJ, Saab PG, Llabre MM, Penedo FJ, McCalla
JR, Schneiderman N. Cardiometabolic risk in adolescents:
associations with physical activity, fitness, and sleep. Ann
Behav Med. 2013 Feb;45(1):121-31.
Daniel LC, Boergers J, Kopel SJ, Koinis-Mitchell D. Missed
sleep and asthma morbidity in urban children. Ann Allergy
Asthma Immunol. 2012 Jul;109(1):41-6.
El-Sheikh M, Buckhalt JA, Granger DA, Erath SA, Acebo C.
The association between children's sleep disruption and
salivary interleukin-6. J Sleep Res. 2007 Jun;16(2):188-
97.
Kieckhefer GM, Ward TM, Tsai SY, Lentz MJ. Nighttime
sleep and daytime nap patterns in school age children with
and without asthma. J Dev Behav Pediatr. 2008
Oct;29(5):338-44.
Martinez-Gomez D, Eisenmann JC, Gomez-Martinez S, Hill
EE, Zapatera B, Veiga OL, Marcos A; AFINOS Study
Group. Sleep duration and emerging cardiometabolic risk
markers in adolescents. The AFINOS study. Sleep Med.
2011 Dec;12(10):997-1002.
Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C,
Ancoli-Israel S, Redline S. Relationships among
sleepiness, sleep time, and psychological functioning in
adolescents. J Pediatr Psychol. 2009 Nov-
Dec;34(10):1175-83.
Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C,
Redline S. Correlates of adolescent sleep time and
variability in sleep time: the role of individual and health
related characteristics. Sleep Med. 2011 Mar;12(3):239-
45.
Pérez de Heredia F, Garaulet M, Gómez-Martínez S, Díaz
LE, Wärnberg J, Androutsos O, Michels N, Breidenassel
C, Cuenca-García M, Huybrechts I, Gottrand F, Ferrari M,
Santaliestra-Pasías AM, Kafatos A, Molnár D, Sjöstrom M,
Widhalm K, Moreno LA, Marcos A; HELENA Study Group.
Self-reported sleep duration, white blood cell counts and
cytokine profiles in European adolescents: the HELENA
study. Sleep Med. 2014 Oct;15(10):1251-8.
Spruyt K, Molfese DL, Gozal D. Sleep duration, sleep
regularity, body weight, and metabolic homeostasis in
school-aged children. Pediatrics. 2011 Feb;127(2):e345-
52.
Tirosh E, Scher A, Sadeh A, Jaffe M, Lavie P. Sleep
characteristics of asthmatics in the first four years of life: a
comparative study. Arch Dis Child. 1993 Apr;68(4):481-3.
Longevity
Aishworiya R, Chan P, Kiing J, Chong SC, Laino AG, Tay
SKh. Sleep behaviour in a sample of preschool children in
Singapore. Ann Acad Med Singapore. 2012 Mar;41(3):99-
104.
Azadbakht L, Kelishadi R, Khodarahmi M, Qorbani M,
Heshmat R, Motlagh ME, Taslimi M, Ardalan G. The
association of sleep duration and cardiometabolic risk
factors in a national sample of children and adolescents:
the CASPIAN III study. Nutrition. 2013 Sep;29(9):1133-41.
Barnes JC, Meldrum RC. The impact of sleep duration on
adolescent development: a genetically informed analysis
of identical twin pairs. J Youth Adolesc. 2015
Feb;44(2):489-506.
Beebe DW, Lewin D, Zeller M, McCabe M, MacLeod K,
Daniels SR, Amin R. Sleep in overweight adolescents:
shorter sleep, poorer sleep quality, sleepiness, and sleep-
disordered breathing. J Pediatr Psychol. 2007 Jan-
Feb;32(1):69-79.
Berentzen NE, Smit HA, Bekkers MB, Brunekreef B,
Koppelman GH, De Jongste JC, Kerkhof M, Van Rossem
L, Wijga AH. Time in bed, sleep quality and associations
with cardiometabolic markers in children: the Prevention
and Incidence of Asthma and Mite Allergy birth cohort
study. J Sleep Res. 2014 Feb;23(1):3-12.
Bibiloni Mdel M, Martinez E, Llull R, Juarez MD, Pons A, Tur
JA. Prevalence and risk factors for obesity in Balearic
Islands adolescents. Br J Nutr. 2010 Jan;103(1):99-106.
Bonuck K, Chervin RD, Howe LD. Sleep-disordered
breathing, sleep duration, and childhood overweight: a
longitudinal cohort study. J Pediatr. 2015 Mar;166(3):632-
9.
Byars KC, Yolton K, Rausch J, Lanphear B, Beebe DW.
Prevalence, patterns, and persistence of sleep problems
in the first 3 years of life. Pediatrics. 2012
Feb;129(2):e276-84.
Chung KF, Cheung MM. Sleep-wake patterns and sleep
disturbance among Hong Kong Chinese adolescents.
Sleep. 2008 Feb;31(2):185-94.
Daniel LC, Boergers J, Kopel SJ, Koinis-Mitchell D. Missed
sleep and asthma morbidity in urban children. Ann Allergy
Asthma Immunol. 2012 Jul;109(1):41-6.
Danielsen YS, Pallesen S, Stormark KM, Nordhus IH,
Bjorvatn B. The relationship between school day sleep
duration and body mass index in Norwegian children
(aged 10-12). Int J Pediatr Obes. 2010 May 3;5(3):214-20.
de Jong E, Stocks T, Visscher TL, HiraSing RA, Seidell JC,
Renders CM. Association between sleep duration and
overweight: the importance of parenting. Int J Obes
(Lond). 2012 Oct;36(10):1278-84.
Do YK, Shin E, Bautista MA, Foo K. The associations
between self-reported sleep duration and adolescent
health outcomes: what is the role of time spent on Internet
use? Sleep Med. 2013 Feb;14(2):195-200.
Drescher AA, Goodwin JL, Silva GE, Quan SF. Caffeine and
screen time in adolescence: associations with short sleep
and obesity. J Clin Sleep Med. 2011 Aug 15;7(4):337-42.
Eaton DK, McKnight-Eily LR, Lowry R, Perry GS, Presley-
Cantrell L, Croft JB. Prevalence of insufficient, borderline,
and optimal hours of sleep among high school students -
United States, 2007. J Adolesc Health. 2010
Apr;46(4):399-401.
Elsenburg LK, Corpeleijn E, van Sluijs EM, Atkin AJ.
Clustering and correlates of multiple health behaviours in
9-10 year old children. PLoS One. 2014;9(6):e99498.
Fitzgerald CT, Messias E, Buysse DJ. Teen sleep and
suicidality: results from the youth risk behavior surveys of
2007 and 2009. J Clin Sleep Med. 2011 Aug 15;7(4):351-
6.
Franco P, Seret N, Van Hees JN, Lanquart JP Jr,
Groswasser J, Kahn A. Cardiac changes during sleep in
sleep-deprived infants. Sleep. 2003 Nov 1;26(7):845-8.
Gau SS, Shang CY, Merikangas KR, Chiu YN, Soong WT,
Cheng AT. Association between morningness-
eveningness and behavioral/emotional problems among
adolescents. J Biol Rhythms. 2007 Jun;22(3):268-74.
Guo X, Zheng L, Li Y, Yu S, Liu S, Zhou X, Zhang X, Sun Z,
Wang R, Sun Y. Association between sleep duration and
hypertension among Chinese children and adolescents.
Clin Cardiol. 2011 Dec;34(12):774-81.
Guo X, Zheng L, Li Y, Yu S, Sun G, Yang H, Zhou X, Zhang
X, Sun Z, Sun Y. Differences in lifestyle behaviors, dietary
habits, and familial factors among normal-weight,
overweight, and obese Chinese children and adolescents.
Int J Behav Nutr Phys Act. 2012 Oct 2;9:120.
Gupta R, Bhatia MS, Chhabra V, Sharma S, Dahiya D,
Semalti K, Sapra R, Dua RS. Sleep patterns of urban
school-going adolescents. Indian Pediatr. 2008
Mar;45(3):183-9.
Hart CN, Cairns A, Jelalian E. Sleep and obesity in children
and adolescents. Pediatr Clin North Am. 2011
Jun;58(3):715-33.
Hjorth MF, Quist JS, Andersen R, Michaelsen KF, Tetens I,
Astrup A, Chaput JP, Sjödin A. Change in sleep duration
and proposed dietary risk factors for obesity in Danish
school children. Pediatr Obes. 2014 Dec;9(6):e156-9.
Jaffa T, Scott S, Hendriks JH, Shapiro CM. ABC of sleep
disorders. Sleep disorders in children. BMJ. 1993 Mar
6;306(6878):640-3.
Jang SI, Lee KS, Park EC. Relationship between current
sleep duration and past suicidal ideation or attempt among
Korean adolescents. J Prev Med Public Health. 2013
Nov;46(6):329-35.
Kang SG, Lee YJ, Kim SJ, Lim W, Lee HJ, Park YM, Cho IH,
Cho SJ, Hong JP. Weekend catch-up sleep is
independently associated with suicide attempts and self-
injury in Korean adolescents. Compr Psychiatry. 2014
Feb;55(2):319-25.
Kjeldsen JS, Hjorth MF, Andersen R, Michaelsen KF, Tetens
I, Astrup A, Chaput JP, Sjödin A. Short sleep duration and
large variability in sleep duration are independently
associated with dietary risk factors for obesity in Danish
school children. Int J Obes (Lond). 2014 Jan;38(1):32-9.
Kleiser C, Schaffrath Rosario A, Mensink GB, Prinz-
Langenohl R, Kurth BM. Potential determinants of obesity
among children and adolescents in Germany: results from
the cross-sectional KiGGS Study. BMC Public Health.
2009 Feb 2;9:46.
Koren D, O'Sullivan KL, Mokhlesi B. Metabolic and glycemic
sequelae of sleep disturbances in children and adults.
Curr Diab Rep. 2015 Jan;15(1):562.
Kuciene R, Dulskiene V. Associations of short sleep duration
with prehypertension and hypertension among Lithuanian
children and adolescents: a cross-sectional study. BMC
Public Health. 2014 Mar 15;14:255.
Kwon JA, Lee M, Yoo KB, Park EC. Does the duration and
time of sleep increase the risk of allergic rhinitis? Results
of the 6-year nationwide Korea youth risk behavior web-
based survey. PLoS One. 2013;8(8):e72507.
Lam LT, Yang L. Short duration of sleep and unintentional
injuries among adolescents in China. Am J Epidemiol.
2007 Nov 1;166(9):1053-8. Epub 2007 Aug 13.
Lazaratou H, Dikeos DG, Anagnostopoulos DC, Sbokou O,
Soldatos CR. Sleep problems in adolescence. A study of
senior high school students in Greece. Eur Child Adolesc
Psychiatry. 2005 Jul;14(4):237-43.
Lee JA, Park HS. Relation between sleep duration,
overweight, and metabolic syndrome in Korean
adolescents. Nutr Metab Cardiovasc Dis. 2014
Jan;24(1):65-71.
Lee YJ, Cho SJ, Cho IH, Kim SJ. Insufficient sleep and
suicidality in adolescents. Sleep. 2012 Apr 1;35(4):455-60.
Li Y, Jin H, Owens JA, Hu C. The association between sleep
and injury among school-aged children in rural China: a
case-control study. Sleep Med. 2008 Jan;9(2):142-8.
Liu X, Uchiyama M, Okawa M, Kurita H. Prevalence and
correlates of self-reported sleep problems among Chinese
adolescents. Sleep. 2000 Feb 1;23(1):27-34.
Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004
Nov 1;27(7):1351-8.
Mak KK, Lee SL, Ho SY, Lo WS, Lam TH. Sleep and
academic performance in Hong Kong adolescents. J Sch
Health. 2012 Nov;82(11):522-7.
Martikainen S, Pesonen AK, Feldt K, Jones A, Lahti J,
Pyhälä R, Heinonen K, Kajantie E, Eriksson J, Räikkönen
K. Poor sleep and cardiovascular function in children.
Hypertension. 2011 Jul;58(1):16-21.
Matamura M, Tochigi M, Usami S, Yonehara H, Fukushima
M, Nishida A, Togo F, Sasaki T. Associations between
sleep habits and mental health status and suicidality in a
longitudinal survey of monozygotic twin adolescents. J
Sleep Res. 2014 Jun;23(3):290-4.
Matricciani LA, Olds TS, Blunden S, Rigney G, Williams MT.
Never enough sleep: a brief history of sleep
recommendations for children. Pediatrics. 2012
Mar;129(3):548-56.
Mitchell JA, Rodriguez D, Schmitz KH, Audrain-McGovern J.
Sleep duration and adolescent obesity. Pediatrics. 2013
May;131(5):e1428-34.
Montgomery-Downs HE, Gozal D. Sleep habits and risk
factors for sleep-disordered breathing in infants and young
toddlers in Louisville, Kentucky. Sleep Med. 2006
Apr;7(3):211-9.
Owens JA, Maxim R, Nobile C, McGuinn M, Msall M.
Parental and self-report of sleep in children with attention-
deficit/hyperactivity disorder. Arch Pediatr Adolesc Med.
2000 Jun;154(6):549-55.
Ozturk A, Mazicioglu M, Poyrazoglu S, Cicek B, Gunay O,
Kurtoglu S. The relationship between sleep duration and
obesity in Turkish children and adolescents. Acta Paediatr.
2009 Apr;98(4):699-702.
Paavonen EJ, Vehkalahti K, Vanhala R, von Wendt L,
Nieminen-von Wendt T, Aronen ET. Sleep in children with
Asperger syndrome. J Autism Dev Disord. 2008
Jan;38(1):41-51.
Padez C, Mourao I, Moreira P, Rosado V. Long sleep
duration and childhood overweight/obesity and body fat.
Am J Hum Biol. 2009 May-Jun;21(3):371-6.
Park JH, Yoo JH, Kim SH. Associations between non-
restorative sleep, short sleep duration and suicidality:
findings from a representative sample of Korean
adolescents. Psychiatry Clin Neurosci. 2013 Jan;67(1):28-
34.
Pizza F, Contardi S, Antognini AB, Zagoraiou M, Borrotti M,
Mostacci B, Mondini S, Cirignotta F. Sleep quality and
motor vehicle crashes in adolescents. J Clin Sleep Med.
2010 Feb 15;6(1):41-5.
Rey-López JP, de Carvalho HB, de Moraes AC, Ruiz JR,
Sjöström M, Marcos A, Polito A, Gottrand F, Manios Y,
Kafatos A, Molnar D, Widhalm K, De Henauw S, Moreno
LA; HELENA study. Sleep time and cardiovascular risk
factors in adolescents: the HELENA (Healthy Lifestyle in
Europe by Nutrition in Adolescence) study. Sleep Med.
2014 Jan;15(1):104-10.
Rutters F, Gerver WJ, Nieuwenhuizen AG, Verhoef SP,
Westerterp-Plantenga MS. Sleep duration and body-
weight development during puberty in a Dutch children
cohort. Int J Obes (Lond). 2010 Oct;34(10):1508-14.
Seicean A, Redline S, Seicean S, Kirchner HL, Gao Y,
Sekine M, Zhu X, Storfer-Isser A. Association between
short sleeping hours and overweight in adolescents:
results from a US Suburban High School survey. Sleep
Breath. 2007 Dec;11(4):285-93.
Shan XY, Xi B, Cheng H, Hou DQ, Wang Y, Mi J.
Prevalence and behavioral risk factors of overweight and
obesity among children aged 2-18 in Beijing, China. Int J
Pediatr Obes. 2010 Oct;5(5):383-9.
Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen
L, Ystrom E, Hysing M. Later emotional and behavioral
problems associated with sleep problems in toddlers: a
longitudinal study. JAMA Pediatr. 2015 Jun;169(6):575-82.
Sivertsen B, Pallesen S, Stormark KM, Bøe T, Lundervold
AJ, Hysing M. Delayed sleep phase syndrome in
adolescents: prevalence and correlates in a large
population based study. BMC Public Health. 2013 Dec
11;13:1163.
Skidmore PM, Howe AS, Polak MA, Wong JE, Lubransky A,
Williams SM, Black KE. Sleep duration and adiposity in
older adolescents from Otago, New Zealand: relationships
differ between boys and girls and are independent of food
choice. Nutr J. 2013 Sep 14;12:128.
Smaldone A, Honig JC, Byrne MW. Sleepless in America:
inadequate sleep and relationships to health and well-
being of our nation's children. Pediatrics. 2007 Feb;119
Suppl 1:S29-37.
Souders MC, Mason TB, Valladares O, Bucan M, Levy SE,
Mandell DS, Weaver TE, Pinto-Martin J. Sleep behaviors
and sleep quality in children with autism spectrum
disorders. Sleep. 2009 Dec;32(12):1566-78.
Stein MA, Mendelsohn J, Obermeyer WH, Amromin J,
Benca R. Sleep and behavior problems in school-aged
children. Pediatrics. 2001 Apr;107(4):E60.
Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP,
Gillman MW. Short sleep duration in infancy and risk of
childhood overweight. Arch Pediatr Adolesc Med. 2008
Apr;162(4):305-11.
Thomas DA, Poole K, McArdle EK, Goodenough PC,
Thompson J, Beardsmore CS, Simpson H. The effect of
sleep deprivation on sleep states, breathing events,
peripheral chemoresponsiveness and arousal propensity
in healthy 3 month old infants. Eur Respir J. 1996
May;9(5):932-8.
Tirosh E, Scher A, Sadeh A, Jaffe M, Lavie P. Sleep
characteristics of asthmatics in the first four years of life: a
comparative study. Arch Dis Child. 1993 Apr;68(4):481-3.
Touchette E, Petit D, Tremblay RE, Boivin M, Falissard B,
Genolini C, Montplaisir JY. Associations between sleep
duration patterns and overweight/obesity at age 6. Sleep.
2008 Nov;31(11):1507-14.
Touchette E, Petit D, Tremblay RE, Montplaisir JY. Risk
factors and consequences of early childhood dyssomnias:
New perspectives. Sleep Med Rev. 2009 Oct;13(5):355-
61.
Wang G, Xu G, Liu Z, Lu N, Ma R, Zhang E. Sleep patterns
and sleep disturbances among Chinese school-aged
children: prevalence and associated factors. Sleep Med.
2013 Jan;14(1):45-52.
Weissbluth M, Brouillete RT, Liu K, Hunt CE. Sleep apnea,
sleep duration, and infant temperament. J Pediatr. 1982
Aug;101(2):307-10.
Winsler A, Deutsch A, Vorona RD, Payne PA, Szklo-Coxe
M. Sleepless in Fairfax: the difference one more hour of
sleep can make for teen hopelessness, suicidal ideation,
and substance use. J Youth Adolesc. 2015 Feb;44(2):362-
78.
Wong WW, Ortiz CL, Lathan D, Moore LA, Konzelmann KL,
Adolph AL, Smith EO, Butte NF. Sleep duration of
underserved minority children in a cross-sectional study.
BMC Public Health. 2013 Jul 12;13:648.
Yang CK, Kim JK, Patel SR, Lee JH. Age-related changes in
sleep/wake patterns among Korean teenagers. Pediatrics.
2005 Jan;115(1 Suppl):250-6.
Yen CF, King BH, Tang TC. The association between short
and long nocturnal sleep durations and risky behaviours
and the moderating factors in Taiwanese adolescents.
Psychiatry Res. 2010 Aug 30;179(1):69-74.
Yen CF, Ko CH, Yen JY, Cheng CP. The multidimensional
correlates associated with short nocturnal sleep duration
and subjective insomnia among Taiwanese adolescents.
Sleep. 2008 Nov;31(11):1515-25.
Mental Health
Accardo JA, Marcus CL, Leonard MB, Shults J, Meltzer LJ,
Elia J. Associations between psychiatric comorbidities and
sleep disturbances in children with attention-
deficit/hyperactivity disorder. J Dev Behav Pediatr. 2012
Feb;33(2):97-105.
Alfano CA, Pina AA, Zerr AA, Villalta IK. Pre-sleep arousal
and sleep problems of anxiety-disordered youth. Child
Psychiatry Hum Dev. 2010 Apr;41(2):156-67.
Arman AR, Ay P, Fis NP, Ersu R, Topuzoglu A, Isik U,
Berkem M. Association of sleep duration with socio-
economic status and behavioural problems among
schoolchildren. Acta Paediatr. 2011 Mar;100(3):420-4.
Aronen ET, Paavonen EJ, Fjällberg M, Soininen M, Törrönen
J. Sleep and psychiatric symptoms in school-age children.
J Am Acad Child Adolesc Psychiatry. 2000 Apr;39(4):502-
8.
Asarnow LD, McGlinchey E, Harvey AG. The effects of
bedtime and sleep duration on academic and emotional
outcomes in a nationally representative sample of
adolescents. J Adolesc Health. 2014 Mar;54(3):350-6.
Astill RG, Van der Heijden KB, Van Ijzendoorn MH, Van
Someren EJ. Sleep, cognition, and behavioral problems in
school-age children: a century of research meta-analyzed.
Psychol Bull. 2012 Nov;138(6):1109-38.
Barnes JC, Meldrum RC. The impact of sleep duration on
adolescent development: a genetically informed analysis
of identical twin pairs. J Youth Adolesc. 2015
Feb;44(2):489-506.
Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW.
Sleep restriction worsens mood and emotion regulation in
adolescents. J Child Psychol Psychiatry. 2014;55(2):180-
90.
Beebe DW, Ris MD, Kramer ME, Long E, Amin R. The
association between sleep disordered breathing,
academic grades, and cognitive and behavioral
functioning among overweight subjects during middle to
late childhood. Sleep. 2010 Nov;33(11):1447-56.
Berger RH, Miller AL, Seifer R, Cares SR, LeBourgeois MK.
Acute sleep restriction effects on emotion responses in 30-
to 36-month-old children. J Sleep Res. 2012
Jun;21(3):235-46.
Biggs SN, Lushington K, van den Heuvel CJ, Martin AJ,
Kennedy JD. Inconsistent sleep schedules and daytime
behavioral difficulties in school-aged children. Sleep Med.
2011 Sep;12(8):780-6.
Burt J, Dube L, Thibault L, Gruber R. Sleep and eating in
childhood: a potential behavioral mechanism underlying
the relationship between poor sleep and obesity. Sleep
Med. 2014 Jan;15(1):71-5.
Capaldi Ii VF, Handwerger K, Richardson E, Stroud LR.
Associations between sleep and cortisol responses to
stress in children and adolescents: a pilot study. Behav
Sleep Med. 2005;3(4):177-92.
Carskadon MA. Sleep in adolescents: the perfect storm.
Pediatr Clin North Am. 2011 Jun;58(3):637-47.
Carvalho Bos S, Gomes A, Clemente V, Marques M, Pereira
AT, Maia B, Soares MJ, Cabral AS, Macedo A, Gozal D,
Azevedo MH. Sleep and behavioral/emotional problems in
children: a population-based study. Sleep Med. 2009
Jan;10(1):66-74.
Cassoff J, Bhatti JA, Gruber R. The effect of sleep restriction
on neurobehavioural functioning in normally developing
children and adolescents: insights from the Attention,
Behaviour and Sleep Laboratory. Pathol Biol (Paris). 2014
Oct;62(5):319-31.
Cortese S, Konofal E, Yateman N, Mouren MC, Lecendreux
M. Sleep and alertness in children with attention-
deficit/hyperactivity disorder: a systematic review of the
literature. Sleep. 2006 Apr;29(4):504-11.
Cortesi F, Giannotti F, Sebastiani T, Vagnoni C, Marioni P.
Cosleeping versus solitary sleeping in children with
bedtime problems: child emotional problems and parental
distress. Behav Sleep Med. 2008;6(2):89-105.
Countryman AJ, Saab PG, Llabre MM, Penedo FJ, McCalla
JR, Schneiderman N. Cardiometabolic risk in adolescents:
associations with physical activity, fitness, and sleep. Ann
Behav Med. 2013 Feb;45(1):121-31.
Dagys N, McGlinchey EL, Talbot LS, Kaplan KA, Dahl RE,
Harvey AG. Double trouble? The effects of sleep
deprivation and chronotype on adolescent affect. J Child
Psychol Psychiatry. 2012 Jun;53(6):660-7.
Dahl RE, Lewin DS. Pathways to adolescent health sleep
regulation and behavior. J Adolesc Health. 2002 Dec;31(6
Suppl):175-84.
Dahl RE, Ryan ND, Matty MK, Birmaher B, al-Shabbout M,
Williamson DE, Kupfer DJ. Sleep onset abnormalities in
depressed adolescents. Biol Psychiatry. 1996 Mar
15;39(6):400-10.
Daniel LC, Boergers J, Kopel SJ, Koinis-Mitchell D. Missed
sleep and asthma morbidity in urban children. Ann Allergy
Asthma Immunol. 2012 Jul;109(1):41-6.
Do YK, Shin E, Bautista MA, Foo K. The associations
between self-reported sleep duration and adolescent
health outcomes: what is the role of time spent on Internet
use? Sleep Med. 2013 Feb;14(2):195-200.
Doane LD, Thurston EC. Associations among sleep, daily
experiences, and loneliness in adolescence: evidence of
moderating and bidirectional pathways. J Adolesc. 2014
Feb;37(2):145-54.
El-Sheikh M, Buckhalt JA, Mark Cummings E, Keller P.
Sleep disruptions and emotional insecurity are pathways
of risk for children. J Child Psychol Psychiatry. 2007
Jan;48(1):88-96.
Ertan P, Yilmaz O, Caglayan M, Sogut A, Aslan S, Yuksel H.
Relationship of sleep quality and quality of life in children
with monosymptomatic enuresis. Child Care Health Dev.
2009 Jul;35(4):469-74.
Fallone G, Acebo C, Seifer R, Carskadon MA. Experimental
restriction of sleep opportunity in children: effects on
teacher ratings. Sleep. 2005 Dec;28(12):1561-7.
Fallone G, Acebo C, Arnedt JT, Seifer R, Carskadon MA.
Effects of acute sleep restriction on behavior, sustained
attention, and response inhibition in children. Percept Mot
Skills. 2001 Aug;93(1):213-29.
Fredriksen K, Rhodes J, Reddy R, Way N. Sleepless in
Chicago: tracking the effects of adolescent sleep loss
during the middle school years. Child Dev. 2004 Jan-
Feb;75(1):84-95.
Gau SS, Shang CY, Merikangas KR, Chiu YN, Soong WT,
Cheng AT. Association between morningness-
eveningness and behavioral/emotional problems among
adolescents. J Biol Rhythms. 2007 Jun;22(3):268-74.
Giannotti F, Cortesi F, Cerquiglini A, Miraglia D, Vagnoni C,
Sebastiani T, Bernabei P. An investigation of sleep
characteristics, EEG abnormalities and epilepsy in
developmentally regressed and non-regressed children
with autism. J Autism Dev Disord. 2008 Nov;38(10):1888-
97.
Gruber R, Cassoff J, Frenette S, Wiebe S, Carrier J. Impact
of sleep extension and restriction on children's emotional
lability and impulsivity. Pediatrics. 2012 Nov;130(5):e1155-
61.
Gruber R, Wiebe S, Montecalvo L, Brunetti B, Amsel R,
Carrier J. Impact of sleep restriction on neurobehavioral
functioning of children with attention deficit hyperactivity
disorder. Sleep. 2011 Mar 1;34(3):315-23.
Gruber R, Xi T, Frenette S, Robert M, Vannasinh P, Carrier
J. Sleep disturbances in prepubertal children with attention
deficit hyperactivity disorder: a home polysomnography
study. Sleep. 2009 Mar;32(3):343-50.
Gruber R, Sadeh A, Raviv A. Instability of sleep patterns in
children with attention-deficit/hyperactivity disorder. J Am
Acad Child Adolesc Psychiatry. 2000 Apr;39(4):495-501.
Hansen M, Janssen I, Schiff A, Zee PC, Dubocovich ML.
The impact of school daily schedule on adolescent sleep.
Pediatrics. 2005 Jun;115(6):1555-61.
Hiscock H, Sciberras E, Mensah F, Gerner B, Efron D,
Khano S, Oberklaid F. Impact of a behavioural sleep
intervention on symptoms and sleep in children with
attention deficit hyperactivity disorder, and parental mental
health: randomised controlled trial. BMJ. 2015 Jan
20;350:h68.
Hodge D, Carollo TM, Lewin M, Hoffman CD, Sweeney DP.
Sleep patterns in children with and without autism
spectrum disorders: developmental comparisons. Res Dev
Disabil. 2014 Jul;35(7):1631-8.
Holley S, Hill CM, Stevenson J. An hour less sleep is a risk
factor for childhood conduct problems. Child Care Health
Dev. 2011 Jul;37(4):563-70.
Honomichl RD, Goodlin-Jones BL, Burnham M, Gaylor E,
Anders TF. Sleep patterns of children with pervasive
developmental disorders. J Autism Dev Disord. 2002
Dec;32(6):553-61.
Humphreys JS, Gringras P, Blair PS, Scott N, Henderson J,
Fleming PJ, Emond AM. Sleep patterns in children with
autistic spectrum disorders: a prospective cohort study.
Arch Dis Child. 2014 Feb;99(2):114-8.
Kang SG, Lee YJ, Kim SJ, Lim W, Lee HJ, Park YM, Cho IH,
Cho SJ, Hong JP. Weekend catch-up sleep is
independently associated with suicide attempts and self-
injury in Korean adolescents. Compr Psychiatry. 2014
Feb;55(2):319-25.
Keller PS, El-Sheikh M, Buckhalt JA. Children's attachment
to parents and their academic functioning: sleep
disruptions as moderators of effects. J Dev Behav Pediatr.
2008 Dec;29(6):441-9.
Kelly RJ, El-Sheikh M. Reciprocal relations between
children's sleep and their adjustment over time. Dev
Psychol. 2014 Apr;50(4):1137-47.
Kim HS, Ham OK, Kim JW, Park JY. Association between
sleep duration and psychological health in overweight and
obese children in Korea. Nurs Health Sci. 2012
Jun;14(2):238-43.
Komada Y, Abe T, Okajima I, Asaoka S, Matsuura N, Usui
A, Shirakawa S, Inoue Y. Short sleep duration and
irregular bedtime are associated with increased behavioral
problems among Japanese preschool-age children.
Tohoku J Exp Med. 2011;224(2):127-36.
Kouros CD, El-Sheikh M. Daily mood and sleep: reciprocal
relations and links with adjustment problems. J Sleep Res.
2015 Feb;24(1):24-31.
Kwon JA, Lee M, Yoo KB, Park EC. Does the duration and
time of sleep increase the risk of allergic rhinitis? Results
of the 6-year nationwide Korea youth risk behavior web-
based survey. PLoS One. 2013;8(8):e72507.
Lee YJ, Cho SJ, Cho IH, Kim SJ. Insufficient sleep and
suicidality in adolescents. Sleep. 2012 Apr 1;35(4):455-60.
Lehto JE, Uusitalo-Malmivaara L. Sleep-related factors:
associations with poor attention and depressive
symptoms. Child Care Health Dev. 2014 May;40(3):419-
25.
Lewandowski AS, Palermo TM, De la Motte S, Fu R.
Temporal daily associations between pain and sleep in
adolescents with chronic pain versus healthy adolescents.
Pain. 2010 Oct;151(1):220-5.
Lin WH, Yi CC. Unhealthy sleep practices, conduct
problems, and daytime functioning during adolescence. J
Youth Adolesc. 2015 Feb;44(2):431-46.
Liu X, Forbes EE, Ryan ND, Rofey D, Hannon TS, Dahl RE.
Rapid eye movement sleep in relation to overweight in
children and adolescents. Arch Gen Psychiatry. 2008
Aug;65(8):924-32.
Liu X, Hubbard JA, Fabes RA, Adam JB. Sleep disturbances
and correlates of children with autism spectrum disorders.
Child Psychiatry Hum Dev. 2006 Winter;37(2):179-91.
Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004
Nov 1;27(7):1351-8.
Liu X, Zhou H. Sleep duration, insomnia and behavioral
problems among Chinese adolescents. Psychiatry Res.
2002 Aug 5;111(1):75-85.
Lytle LA, Pasch KE, Farbakhsh K. The relationship between
sleep and weight in a sample of adolescents. Obesity
(Silver Spring). 2011 Feb;19(2):324-31.
Magee CA, Gordon R, Caputi P. Distinct developmental
trends in sleep duration during early childhood. Pediatrics.
2014 Jun;133(6):e1561-7.
Malow BA, Marzec ML, McGrew SG, Wang L, Henderson
LM, Stone WL. Characterizing sleep in children with
autism spectrum disorders: a multidimensional approach.
Sleep. 2006 Dec;29(12):1563-71.
Maski KP, Kothare SV. Sleep deprivation and
neurobehavioral functioning in children. Int J
Psychophysiol. 2013 Aug;89(2):259-64.
Matamura M, Tochigi M, Usami S, Yonehara H, Fukushima
M, Nishida A, Togo F, Sasaki T. Associations between
sleep habits and mental health status and suicidality in a
longitudinal survey of monozygotic twin adolescents. J
Sleep Res. 2014 Jun;23(3):290-4.
Matsushita M, Koyama A, Ushijima H, Mikami A, Katsumata
Y, Kikuchi Y, Ichimi N, Jono T, Fujise N, Ikeda M. Sleep
duration and its association with sleepiness and
depression in ronin-sei" preparatory school students."
Asian J Psychiatr. 2014 Jun;9:61-6.
McDermott BM, Mamun AA, Najman JM, Williams GM,
O'callaghan MJ, Bor W. Preschool children perceived by
mothers as irregular eaters: physical and psychosocial
predictors from a birth cohort study. J Dev Behav Pediatr.
2008 Jun;29(3):197-205.
Meltzer LJ, Mindell JA. Sleep and sleep disorders in children
and adolescents. Psychiatr Clin North Am. 2006
Dec;29(4):1059-76
Mercier L, Pivik RT, Busby K. Sleep patterns in reading
disabled children. Sleep. 1993 Apr;16(3):207-15.
Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C,
Redline S. Correlates of adolescent sleep time and
variability in sleep time: the role of individual and health
related characteristics. Sleep Med. 2011 Mar;12(3):239-
45.
Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C,
Ancoli-Israel S, Redline S. Relationships among
sleepiness, sleep time, and psychological functioning in
adolescents. J Pediatr Psychol. 2009 Nov-
Dec;34(10):1175-83.
Moseley L, Gradisar M. Evaluation of a school-based
intervention for adolescent sleep problems. Sleep. 2009
Mar;32(3):334-41.
Owens J. Classification and epidemiology of childhood sleep
disorders. Prim Care. 2008 Sep;35(3):533-46, vii.
Owens JA, Belon K, Moss P. Impact of delaying school start
time on adolescent sleep, mood, and behavior. Arch
Pediatr Adolesc Med. 2010 Jul;164(7):608-14.
Owens JA, Fernando S, Mc Guinn M. Sleep disturbance and
injury risk in young children. Behav Sleep Med.
2005;3(1):18-31.
Owens JA, Maxim R, Nobile C, McGuinn M, Msall M.
Parental and self-report of sleep in children with attention-
deficit/hyperactivity disorder. Arch Pediatr Adolesc Med.
2000 Jun;154(6):549-55.
Paavonen EJ, Räikkönen K, Lahti J, Komsi N, Heinonen K,
Pesonen AK, Järvenpää AL, Strandberg T, Kajantie E,
Porkka-Heiskanen T. Short sleep duration and behavioral
symptoms of attention-deficit/hyperactivity disorder in
healthy 7- to 8-year-old children. Pediatrics. 2009
May;123(5):e857-64.
Paavonen EJ, Porkka-Heiskanen T, Lahikainen AR. Sleep
quality, duration and behavioral symptoms among 5-6-
year-old children. Eur Child Adolesc Psychiatry. 2009
Dec;18(12):747-54.
Paavonen EJ, Vehkalahti K, Vanhala R, von Wendt L,
Nieminen-von Wendt T, Aronen ET. Sleep in children with
Asperger syndrome. J Autism Dev Disord. 2008
Jan;38(1):41-51
Paavonen EJ, Nieminen-von Wendt T, Vanhala R, Aronen
ET, von Wendt L. Effectiveness of melatonin in the
treatment of sleep disturbances in children with Asperger
disorder. J Child Adolesc Psychopharmacol. 2003
Spring;13(1):83-95.
Paciência I, Barros H, Araújo J, Ramos E. Association
between sleep duration and blood pressure in
adolescents. Hypertens Res. 2013 Aug;36(8):747-52.
Pantic I, Damjanovic A, Todorovic J, Topalovic D, Bojovic-
Jovic D, Ristic S, Pantic S. Association between online
social networking and depression in high school students:
behavioral physiology viewpoint. Psychiatr Danub. 2012
Mar;24(1):90-3.
Pasch KE, Laska MN, Lytle LA, Moe SG. Adolescent sleep,
risk behaviors, and depressive symptoms: are they linked?
Am J Health Behav. 2010 Mar-Apr;34(2):237-48.
Perez-Chada D, Perez-Lloret S, Videla AJ, Cardinali D,
Bergna MA, Fernändez-Acquier M, Larrateguy L, Zabert
GE, Drake C. Sleep disordered breathing and daytime
sleepiness are associated with poor academic
performance in teenagers. A study using the Pediatric
Daytime Sleepiness Scale (PDSS). Sleep. 2007
Dec;30(12):1698-703.
Perkinson-Gloor N, Lemola S, Grob A. Sleep duration,
positive attitude toward life, and academic achievement:
the role of daytime tiredness, behavioral persistence, and
school start times. J Adolesc. 2013 Apr;36(2):311-8.
Roberts RE, Duong HT. The prospective association
between sleep deprivation and depression among
adolescents. Sleep. 2014 Feb 1;37(2):239-44.
Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral
functioning, and behavior problems in school-age children.
Child Dev. 2002 Mar-Apr;73(2):405-17.
Scharf RJ, Demmer RT, Silver EJ, Stein RE. Nighttime sleep
duration and externalizing behaviors of preschool children.
J Dev Behav Pediatr. 2013 Jul-Aug;34(6):384-91.
Schreck KA, Mulick JA, Smith AF. Sleep problems as
possible predictors of intensified symptoms of autism. Res
Dev Disabil. 2004 Jan-Feb;25(1):57-66.
Scott N, Blair PS, Emond AM, Fleming PJ, Humphreys JS,
Henderson J, Gringras P. Sleep patterns in children with
ADHD: a population-based cohort study from birth to
11 years. J Sleep Res. 2013 Apr;22(2):121-8.
Segura-Jiménez V, Carbonell-Baeza A, Keating XD, Ruiz
JR, Castro-Piñero J. Association of sleep patterns with
psychological positive health and health complaints in
children and adolescents. Qual Life Res. 2015
Apr;24(4):885-95.
Short MA, Gradisar M, Lack LC, Wright HR, Dohnt H. The
sleep patterns and well-being of Australian adolescents. J
Adolesc. 2013 Feb;36(1):103-10.
Short MA, Gradisar M, Lack LC, Wright HR. The impact of
sleep on adolescent depressed mood, alertness and
academic performance. J Adolesc. 2013 Dec;36(6):1025-
33.
Shur-Fen Gau S. Prevalence of sleep problems and their
association with inattention/hyperactivity among children
aged 6-15 in Taiwan. J Sleep Res. 2006 Dec;15(4):403-
14. Erratum in: J Sleep Res. 2010 Jun;19(2):379. Shur-
Fen, Gau Susan [corrected to Shur-Fen Gau, Susan].
Silva GE, Goodwin JL, Parthasarathy S, Sherrill DL, Vana
KD, Drescher AA, Quan SF. Longitudinal association
between short sleep, body weight, and emotional and
learning problems in Hispanic and Caucasian children.
Sleep. 2011 Sep 1;34(9):1197-205.
Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen
L, Ystrom E, Hysing M. Later emotional and behavioral
problems associated with sleep problems in toddlers: a
longitudinal study. JAMA Pediatr. 2015 Jun;169(6):575-82.
Sivertsen B, Harvey AG, Lundervold AJ, Hysing M. Sleep
problems and depression in adolescence: results from a
large population-based study of Norwegian adolescents
aged 16-18 years. Eur Child Adolesc Psychiatry. 2014
Aug;23(8):681-9.
Smaldone A, Honig JC, Byrne MW. Sleepless in America:
inadequate sleep and relationships to health and well-
being of our nation's children. Pediatrics. 2007 Feb;119
Suppl 1:S29-37.
Souders MC, Mason TB, Valladares O, Bucan M, Levy SE,
Mandell DS, Weaver TE, Pinto-Martin J. Sleep behaviors
and sleep quality in children with autism spectrum
disorders. Sleep. 2009 Dec;32(12):1566-78.
Spruyt K, Gozal D. Sleep disturbances in children with
attention-deficit/hyperactivity disorder. Expert Rev
Neurother. 2011 Apr;11(4):565-77.
Stein MA, Mendelsohn J, Obermeyer WH, Amromin J,
Benca R. Sleep and behavior problems in school-aged
children. Pediatrics. 2001 Apr;107(4):E60.
Suzuki H, Kaneita Y, Osaki Y, Minowa M, Kanda H, Suzuki
K, Wada K, Hayashi K, Tanihata T, Ohida T. Clarification
of the factor structure of the 12-item General Health
Questionnaire among Japanese adolescents and
associated sleep status. Psychiatry Res. 2011 Jun
30;188(1):138-46.
Tininenko JR, Fisher PA, Bruce J, Pears KC. Associations
between sleep and inattentive/hyperactive problem
behavior among foster and community children. J Dev
Behav Pediatr. 2010 Oct;31(8):668-74.
Touchette E, Petit D, Tremblay RE, Montplaisir JY. Risk
factors and consequences of early childhood dyssomnias:
New perspectives. Sleep Med Rev. 2009 Oct;13(5):355-
61.
Touchette E, Côté SM, Petit D, Liu X, Boivin M, Falissard B,
Tremblay RE, Montplaisir JY. Short nighttime sleep-
duration and hyperactivity trajectories in early childhood.
Pediatrics. 2009 Nov;124(5):e985-93.
Vazsonyi AT, Harris C, Terveer AM, Pagava K, Phagava H,
Michaud PA. Parallel mediation effects by sleep on the
parental warmth-problem behavior links: evidence from
national probability samples of Georgian and Swiss
adolescents. J Youth Adolesc. 2015 Feb;44(2):331-45.
Vriend JL, Davidson FD, Corkum PV, Rusak B, Chambers
CT, McLaughlin EN. Manipulating sleep duration alters
emotional functioning and cognitive performance in
children. J Pediatr Psychol. 2013 Nov;38(10):1058-69.
Ward TM, Gay C, Alkon A, Anders TF, Lee KA. Nocturnal
sleep and daytime nap behaviors in relation to salivary
cortisol levels and temperament in preschool-age children
attending child care. Biol Res Nurs. 2008 Jan;9(3):244-53.
Wiggs L, Stores G. Behavioural treatment for sleep problems
in children with severe learning disabilities and challenging
daytime behaviour: effect on daytime behaviour. J Child
Psychol Psychiatry. 1999 May;40(4):627-35.
Willoughby MT, Angold A, Egger HL. Parent-reported
attention-deficit/hyperactivity disorder symptomatology
and sleep problems in a preschool-age pediatric clinic
sample. J Am Acad Child Adolesc Psychiatry. 2008
Sep;47(9):1086-94.
Winsler A, Deutsch A, Vorona RD, Payne PA, Szklo-Coxe
M. Sleepless in Fairfax: the difference one more hour of
sleep can make for teen hopelessness, suicidal ideation,
and substance use. J Youth Adolesc. 2015 Feb;44(2):362-
78.
Yen CF, King BH, Tang TC. The association between short
and long nocturnal sleep durations and risky behaviours
and the moderating factors in Taiwanese adolescents.
Psychiatry Res. 2010 Aug 30;179(1):69-74.
Yen CF, Ko CH, Yen JY, Cheng CP. The multidimensional
correlates associated with short nocturnal sleep duration
and subjective insomnia among Taiwanese adolescents.
Sleep. 2008 Nov;31(11):1515-25.
Yip T. The effects of ethnic/racial discrimination and sleep
quality on depressive symptoms and self-esteem
trajectories among diverse adolescents. J Youth Adolesc.
2015 Feb;44(2):419-30.
Yokomaku A, Misao K, Omoto F, Yamagishi R, Tanaka K,
Takada K, Kohyama J. A study of the association between
sleep habits and problematic behaviors in preschool
children. Chronobiol Int. 2008 Jul;25(4):549-64.
Metabolic Health
Agras WS, Hammer LD, McNicholas F, Kraemer HC. Risk
factors for childhood overweight: a prospective study from
birth to 9.5 years. J Pediatr. 2004 Jul;145(1):20-5. Erratum
in: J Pediatr. 2004 Sep;145(3):424.
Al-Disi D, Al-Daghri N, Khanam L, Al-Othman A, Al-Saif M,
Sabico S, Chrousos G. Subjective sleep duration and
quality influence diet composition and circulating
adipocytokines and ghrelin levels in teen-age girls. Endocr
J. 2010;57(10):915-23.
Al-Hazzaa HM, Musaiger AO, Abahussain NA, Al-Sobayel
HI, Qahwaji DM. Lifestyle correlates of self-reported sleep
duration among Saudi adolescents: a multicentre school-
based cross-sectional study. Child Care Health Dev. 2014
Jul;40(4):533-42.
Altenburg TM, Chinapaw MJ, van der Knaap ET, Brug J,
Manios Y, Singh AS. Longer sleep--slimmer kids: the
ENERGY-project. PLoS One. 2013;8(3):e59522.
Androutsos O, Moschonis G, Mavrogianni C, Roma-
Giannikou E, Chrousos GP, Kanaka-Gantenbein C,
Manios Y. Identification of lifestyle patterns, including
sleep deprivation, associated with insulin resistance in
children: the Healthy Growth Study. Eur J Clin Nutr. 2014
Mar;68(3):344-9.
Appelhans BM, Fitzpatrick SL, Li H, Cail V, Waring ME,
Schneider KL, Whited MC, Busch AM, Pagoto SL. The
home environment and childhood obesity in low-income
households: indirect effects via sleep duration and screen
time. BMC Public Health. 2014 Nov 9;14:1160.
Arora T, Taheri S. Associations among late chronotype,
body mass index and dietary behaviors in young
adolescents. Int J Obes (Lond). 2015 Jan;39(1):39-44.
Arora T, Hussain S, Hubert Lam KB, Lily Yao G, Neil
Thomas G, Taheri S. Exploring the complex pathways
among specific types of technology, self-reported sleep
duration and body mass index in UK adolescents. Int J
Obes (Lond). 2013 Sep;37(9):1254-60.
Arora T, Hosseini-Araghi M, Bishop J, Yao GL, Thomas GN,
Taheri S. The complexity of obesity in U.K. adolescents:
relationships with quantity and type of technology, sleep
duration and quality, academic performance and
aspiration. Pediatr Obes. 2013 Oct;8(5):358-66.
Azadbakht L, Kelishadi R, Khodarahmi M, Qorbani M,
Heshmat R, Motlagh ME, Taslimi M, Ardalan G. The
association of sleep duration and cardiometabolic risk
factors in a national sample of children and adolescents:
the CASPIAN III study. Nutrition. 2013 Sep;29(9):1133-41.
Ball GD, Lenk JM, Barbarich BN, Plotnikoff RC, Fishburne
GJ, Mackenzie KA, Willows ND. Overweight children and
adolescents referred for weight management: are they
meeting lifestyle behaviour recommendations? Appl
Physiol Nutr Metab. 2008 Oct;33(5):936-45.
Beebe DW, Ris MD, Kramer ME, Long E, Amin R. The
association between sleep disordered breathing,
academic grades, and cognitive and behavioral
functioning among overweight subjects during middle to
late childhood. Sleep. 2010 Nov;33(11):1447-56.
Beebe DW, Lewin D, Zeller M, McCabe M, MacLeod K,
Daniels SR, Amin R. Sleep in overweight adolescents:
shorter sleep, poorer sleep quality, sleepiness, and sleep-
disordered breathing. J Pediatr Psychol. 2007 Jan-
Feb;32(1):69-79.
Bell JF, Zimmerman FJ. Shortened nighttime sleep duration
in early life and subsequent childhood obesity. Arch
Pediatr Adolesc Med. 2010 Sep;164(9):840-5. Erratum in:
Arch Pediatr Adolesc Med. 2010 Nov;164(11):1070.
Bibiloni Mdel M, Martinez E, Llull R, Juarez MD, Pons A, Tur
JA. Prevalence and risk factors for obesity in Balearic
Islands adolescents. Br J Nutr. 2010 Jan;103(1):99-106.
Bonuck K, Chervin RD, Howe LD. Sleep-disordered
breathing, sleep duration, and childhood overweight: a
longitudinal cohort study. J Pediatr. 2015 Mar;166(3):632-
9.
Brandalize M, Pereira RF, Leite N, Filho GL, Louzada FM.
Effect of morning school schedule on sleep and
anthropometric variables in adolescents: a follow-up study.
Chronobiol Int. 2011 Nov;28(9):779-85
Burt J, Dube L, Thibault L, Gruber R. Sleep and eating in
childhood: a potential behavioral mechanism underlying
the relationship between poor sleep and obesity. Sleep
Med. 2014 Jan;15(1):71-5.
Börnhorst C, Hense S, Ahrens W, Hebestreit A, Reisch L,
Barba G, von Kries R, Bayer O; IDEFICS Consortium.
From sleep duration to childhood obesity--what are the
pathways? Eur J Pediatr. 2012 Jul;171(7):1029-38.
Calamaro CJ, Park S, Mason TB, Marcus CL, Weaver TE,
Pack A, Ratcliffe SJ. Shortened sleep duration does not
predict obesity in adolescents. J Sleep Res. 2010
Dec;19(4):559-66.
Carrillo-Larco RM, Bernabé-Ortiz A, Miranda JJ. Short sleep
duration and childhood obesity: cross-sectional analysis in
Peru and patterns in four developing countries. PLoS One.
2014;9(11):e112433.
Casazza K, Hanks LJ, Fernandez JR. Shorter sleep may be
a risk factor for impaired bone mass accrual in childhood.
J Clin Densitom. 2011 Oct-Dec;14(4):453-7.
Cassoff J, Bhatti JA, Gruber R. The effect of sleep restriction
on neurobehavioural functioning in normally developing
children and adolescents: insights from the Attention,
Behaviour and Sleep Laboratory. Pathol Biol (Paris). 2014
Oct;62(5):319-31.
Cespedes EM, Rifas-Shiman SL, Redline S, Gillman MW,
Peña MM, Taveras EM. Longitudinal associations of sleep
curtailment with metabolic risk in mid-childhood. Obesity
(Silver Spring). 2014 Dec;22(12):2586-92.
Chamorro R, Algarín C, Garrido M, Causa L, Held C, Lozoff
B, Peirano P. Night time sleep macrostructure is altered in
otherwise healthy 10-year-old overweight children. Int J
Obes (Lond). 2014 Aug;38(8):1120-5.
Chaput JP, Lambert M, Gray-Donald K, McGrath JJ,
Tremblay MS, O'Loughlin J, Tremblay A. Short sleep
duration is independently associated with overweight and
obesity in Quebec children. Can J Public Health. 2011
Sep-Oct;102(5):369-74.
Chaput JP, Brunet M, Tremblay A. Relationship between
short sleeping hours and childhood overweight/obesity:
results from the 'Québec en Forme' Project. Int J Obes
(Lond). 2006 Jul;30(7):1080-5.
Chen X, Beydoun MA, Wang Y. Is sleep duration associated
with childhood obesity? A systematic review and meta-
analysis. Obesity (Silver Spring). 2008 Feb;16(2):265-74.
Cicek B, Ozturk A, Mazicioglu MM, Elmali F, Turp N,
Kurtoglu S. The risk analysis of arm fat area in Turkish
children and adolescents. Ann Hum Biol. 2009 Jan-
Feb;36(1):28-37.
Countryman AJ, Saab PG, Llabre MM, Penedo FJ, McCalla
JR, Schneiderman N. Cardiometabolic risk in adolescents:
associations with physical activity, fitness, and sleep. Ann
Behav Med. 2013 Feb;45(1):121-31.
D'Aniello R, Troisi J, D'Amico O, Sangermano M, Massa G,
Moccaldo A, Pierri L, Poeta M, Vajro P. Emerging
pathomechanisms involved in obesity. J Pediatr
Gastroenterol Nutr. 2015 Jan;60(1):113-9.
Danielsen YS, Pallesen S, Stormark KM, Nordhus IH,
Bjorvatn B. The relationship between school day sleep
duration and body mass index in Norwegian children
(aged 10-12). Int J Pediatr Obes. 2010 May 3;5(3):214-20.
de Jong E, Stocks T, Visscher TL, HiraSing RA, Seidell JC,
Renders CM. Association between sleep duration and
overweight: the importance of parenting. Int J Obes
(Lond). 2012 Oct;36(10):1278-84.
Dev DA, McBride BA, Fiese BH, Jones BL, Cho H; Behalf Of
The Strong Kids Research Team. Risk factors for
overweight/obesity in preschool children: an ecological
approach. Child Obes. 2013 Oct;9(5):399-408.
Diethelm K, Bolzenius K, Cheng G, Remer T, Buyken AE.
Longitudinal associations between reported sleep duration
in early childhood and the development of body mass
index, fat mass index and fat free mass index until age 7.
Int J Pediatr Obes. 2011 Jun;6(2-2):e114-23.
Do YK, Shin E, Bautista MA, Foo K. The associations
between self-reported sleep duration and adolescent
health outcomes: what is the role of time spent on Internet
use? Sleep Med. 2013 Feb;14(2):195-200.
Drescher AA, Goodwin JL, Silva GE, Quan SF. Caffeine and
screen time in adolescence: associations with short sleep
and obesity. J Clin Sleep Med. 2011 Aug 15;7(4):337-42.
Duncan JS, Schofield G, Duncan EK, Rush EC. Risk factors
for excess body fatness in New Zealand children. Asia
Pac J Clin Nutr. 2008;17(1):138-47.
Eisenmann JC, Ekkekakis P, Holmes M. Sleep duration and
overweight among Australian children and adolescents.
Acta Paediatr. 2006 Aug;95(8):956-63.
Ekstedt M, Nyberg G, Ingre M, Ekblom ö, Marcus C. Sleep,
physical activity and BMI in six to ten-year-old children
measured by accelerometry: a cross-sectional study. Int J
Behav Nutr Phys Act. 2013 Jun 22;10:82.
Fatima Y, Doi SA, Mamun AA. Longitudinal impact of sleep
on overweight and obesity in children and adolescents: a
systematic review and bias-adjusted meta-analysis. Obes
Rev. 2015 Feb;16(2):137-49.
Firouzi S, Poh BK, Ismail MN, Sadeghilar A. Sleep habits,
food intake, and physical activity levels in normal and
overweight and obese Malaysian children. Obes Res Clin
Pract. 2014 Jan-Feb;8(1):e70-8.
Fisher A, McDonald L, van Jaarsveld CH, Llewellyn C, Fildes
A, Schrempft S, Wardle J. Sleep and energy intake in
early childhood. Int J Obes (Lond). 2014 Jul;38(7):926-9.
Flint J, Kothare SV, Zihlif M, Suarez E, Adams R, Legido A,
De Luca F. Association between inadequate sleep and
insulin resistance in obese children. J Pediatr. 2007
Apr;150(4):364-9.
Garaulet M, Ortega FB, Ruiz JR, Rey-López JP, Béghin L,
Manios Y, Cuenca-García M, Plada M, Diethelm K,
Kafatos A, Molnár D, Al-Tahan J, Moreno LA. Short sleep
duration is associated with increased obesity markers in
European adolescents: effect of physical activity and
dietary habits. The HELENA study. Int J Obes (Lond).
2011 Oct;35(10):1308-17.
Golley RK, Maher CA, Matricciani L, Olds TS. Sleep duration
or bedtime? Exploring the association between sleep
timing behaviour, diet and BMI in children and
adolescents. Int J Obes (Lond). 2013 Apr;37(4):546-51.
Gozal D, Kheirandish-Gozal L. Childhood obesity and sleep:
relatives, partners, or both?--a critical perspective on the
evidence. Ann N Y Acad Sci. 2012 Aug;1264:135-41.
Graef DM, Janicke DM, McCrae CS. Sleep patterns of a
primarily obese sample of treatment-seeking children. J
Clin Sleep Med. 2014 Oct 15;10(10):1111-7
Guo X, Zheng L, Li Y, Yu S, Sun G, Yang H, Zhou X, Zhang
X, Sun Z, Sun Y. Differences in lifestyle behaviors, dietary
habits, and familial factors among normal-weight,
overweight, and obese Chinese children and adolescents.
Int J Behav Nutr Phys Act. 2012 Oct 2;9:120.
Haines J, McDonald J, O'Brien A, Sherry B, Bottino CJ,
Schmidt ME, Taveras EM. Healthy Habits, Happy Homes:
randomized trial to improve household routines for obesity
prevention among preschool-aged children. JAMA Pediatr.
2013 Nov;167(11):1072-9.
Hart CN, Carskadon MA, Considine RV, Fava JL, Lawton J,
Raynor HA, Jelalian E, Owens J, Wing R. Changes in
children's sleep duration on food intake, weight, and leptin.
Pediatrics. 2013 Dec;132(6):e1473-80.
Hart CN, Cairns A, Jelalian E. Sleep and obesity in children
and adolescents. Pediatr Clin North Am. 2011 Jun;58(3):
715-33.
Hart CN, Jelalian E. Shortened sleep duration is associated
with pediatric overweight. Behav Sleep Med.
2008;6(4):251-67.
Hassan F, Davis MM, Chervin RD. No independent
association between insufficient sleep and childhood
obesity in the National Survey of Children's Health. J Clin
Sleep Med. 2011 Apr 15;7(2):153-7.
Hense S, Pohlabeln H, De Henauw S, Eiben G, Molnar D,
Moreno LA, Barba G, Hadjigeorgiou C, Veidebaum T,
Ahrens W. Sleep duration and overweight in European
children: is the association modified by geographic region?
Sleep. 2011 Jul 1;34(7):885-90.
Hiscock H, Scalzo K, Canterford L, Wake M. Sleep duration
and body mass index in 0-7-year olds. Arch Dis Child.
2011 Aug;96(8):735-9.
Hjorth MF, Chaput JP, Ritz C, Dalskov SM, Andersen R,
Astrup A, Tetens I, Michaelsen KF, Sjödin A. Fatness
predicts decreased physical activity and increased
sedentary time, but not vice versa: support from a
longitudinal study in 8- to 11-year-old children. Int J Obes
(Lond). 2014 Jul;38(7):959-65.
Hjorth MF, Quist JS, Andersen R, Michaelsen KF, Tetens I,
Astrup A, Chaput JP, Sjödin A. Change in sleep duration
and proposed dietary risk factors for obesity in Danish
school children. Pediatr Obes. 2014 Dec;9(6):e156-9.
Iglayreger HB, Peterson MD, Liu D, Parker CA, Woolford SJ,
Sallinen Gafka BJ, Hassan F, Gordon PM. Sleep duration
predicts cardiometabolic risk in obese adolescents. J
Pediatr. 2014 May;164(5):1085-1090.e1.
Jarrin DC, McGrath JJ, Poirier P, Quality Cohort
Collaborative Group. Autonomic dysfunction: a possible
pathophysiological pathway underlying the association
between sleep and obesity in children at-risk for obesity. J
Youth Adolesc. 2015 Feb;44(2):285-97.
Jarrin DC, McGrath JJ, Drake CL. Beyond sleep duration:
distinct sleep dimensions are associated with obesity in
children and adolescents. Int J Obes (Lond). 2013
Apr;37(4):552-8.
Javaheri S, Storfer-Isser A, Rosen CL, Redline S.
Association of short and long sleep durations with insulin
sensitivity in adolescents. J Pediatr. 2011 Apr;158(4):617-
23.
Jenni OG, Molinari L, Caflisch JA, Largo RH. Sleep duration
from ages 1 to 10 years: variability and stability in
comparison with growth. Pediatrics. 2007
Oct;120(4):e769-76.
Jiang F, Zhu S, Yan C, Jin X, Bandla H, Shen X. Sleep and
obesity in preschool children. J Pediatr. 2009
Jun;154(6):814-8.
Jiang YR, Spruyt K, Chen WJ, Shen XM, Jiang F. Somatic
growth of lean children: the potential role of sleep. World J
Pediatr. 2014 Aug;10(3):245-50.
Jones CH, Pollard TM, Summerbell CD, Ball H. Could
parental rules play a role in the association between short
sleep and obesity in young children? J Biosoc Sci. 2014
May;46(3):405-18.
Kim HS, Ham OK, Kim JW, Park JY. Association between
sleep duration and psychological health in overweight and
obese children in Korea. Nurs Health Sci. 2012
Jun;14(2):238-43.
Kjeldsen JS, Hjorth MF, Andersen R, Michaelsen KF, Tetens
I, Astrup A, Chaput JP, Sjödin A. Short sleep duration and
large variability in sleep duration are independently
associated with dietary risk factors for obesity in Danish
school children. Int J Obes (Lond). 2014 Jan;38(1):32-9.
Kleiser C, Schaffrath Rosario A, Mensink GB, Prinz-
Langenohl R, Kurth BM. Potential determinants of obesity
among children and adolescents in Germany: results from
the cross-sectional KiGGS Study. BMC Public Health.
2009 Feb 2;9:46.
Klingenberg L, Christensen LB, Hjorth MF, Zangenberg S,
Chaput JP, Sjödin A, Mølgaard C, Michaelsen KF. No
relation between sleep duration and adiposity indicators in
9-36 months old children: the SKOT cohort. Pediatr Obes.
2013 Feb;8(1):e14-8.
Klingenberg L, Chaput JP, Holmbäck U, Jennum P, Astrup
A, Sjödin A. Sleep restriction is not associated with a
positive energy balance in adolescent boys. Am J Clin
Nutr. 2012 Aug;96(2):240-8.
Knutson KL. Sex differences in the association between
sleep and body mass index in adolescents. J Pediatr.
2005 Dec;147(6):830-4.
Koren D, O'Sullivan KL, Mokhlesi B. Metabolic and glycemic
sequelae of sleep disturbances in children and adults.
Curr Diab Rep. 2015 Jan;15(1):562.
Koren D, Levitt Katz LE, Brar PC, Gallagher PR, Berkowitz
RI, Brooks LJ. Sleep architecture and glucose and insulin
homeostasis in obese adolescents. Diabetes Care. 2011
Nov;34(11):2442-7.
Kuriyan R, Bhat S, Thomas T, Vaz M, Kurpad AV. Television
viewing and sleep are associated with overweight among
urban and semi-urban South Indian children. Nutr J. 2007
Sep 20;6:25.
Landis AM, Parker KP, Dunbar SB. Sleep, hunger, satiety,
food cravings, and caloric intake in adolescents. J Nurs
Scholarsh. 2009;41(2):115-23.
Lee JA, Park HS. Relation between sleep duration,
overweight, and metabolic syndrome in Korean
adolescents. Nutr Metab Cardiovasc Dis. 2014
Jan;24(1):65-71.
Lehto R, Ray C, Lahti-Koski M, Roos E. Health behaviors,
waist circumference and waist-to-height ratio in children.
Eur J Clin Nutr. 2011 Jul;65(7):841-8.
Leproult R, Van Cauter E. Role of sleep and sleep loss in
hormonal release and metabolism. Endocr Dev.
2010;17:11-21.
Liu J, Zhang A, Li L. Sleep duration and overweight/obesity
in children: review and implications for pediatric nursing. J
Spec Pediatr Nurs. 2012 Jul;17(3):193-204.
Liu X, Forbes EE, Ryan ND, Rofey D, Hannon TS, Dahl RE.
Rapid eye movement sleep in relation to overweight in
children and adolescents. Arch Gen Psychiatry. 2008
Aug;65(8):924-32.
Lumeng JC, Somashekar D, Appugliese D, Kaciroti N,
Corwyn RF, Bradley RH. Shorter sleep duration is
associated with increased risk for being overweight at
ages 9 to 12 years. Pediatrics. 2007 Nov;120(5):1020-9.
Lytle LA, Murray DM, Laska MN, Pasch KE, Anderson SE,
Farbakhsh K. Examining the longitudinal relationship
between change in sleep and obesity risk in adolescents.
Health Educ Behav. 2013 Jun;40(3):362-70.
Lytle LA, Pasch KE, Farbakhsh K. The relationship between
sleep and weight in a sample of adolescents. Obesity
(Silver Spring). 2011 Feb;19(2):324-31.
Magee CA, Caputi P, Iverson DC. The longitudinal
relationship between sleep duration and body mass index
in children: a growth mixture modeling approach. J Dev
Behav Pediatr. 2013 Apr;34(3):165-73.
Mahler B, Kamperis K, Schroeder M, Frøkiær J, Djurhuus
JC, Rittig S. Sleep deprivation induces excess diuresis
and natriuresis in healthy children. Am J Physiol Renal
Physiol. 2012 Jan 15;302(2):F236-43.
Martinez SM, Greenspan LC, Butte NF, Gregorich SE, De
Groat CL, Deardorff J, Penilla C, Pasch LA, Flores E,
Tschann JM. Mother-reported sleep, accelerometer-
estimated sleep and weight status in Mexican American
children: sleep duration is associated with increased
adiposity and risk for overweight/obese status. J Sleep
Res. 2014 Jun;23(3):326-34.
Martinez-Gomez D, Eisenmann JC, Gomez-Martinez S, Hill
EE, Zapatera B, Veiga OL, Marcos A; AFINOS Study
Group. Sleep duration and emerging cardiometabolic risk
markers in adolescents. The AFINOS study. Sleep Med.
2011 Dec;12(10):997-1002.
Martinez-Gomez D, Moreno LA, Romeo J, Rey-López P,
Castillo R, Cabero MJ, Vicente-Rodriguez G, Gutiérrez A,
Veiga OL. Combined influence of lifestyle risk factors on
body fat in Spanish adolescents--the Avena study. Obes
Facts. 2011;4(2):105-11.
Matthews KA, Dahl RE, Owens JF, Lee L, Hall M. Sleep
duration and insulin resistance in healthy black and white
adolescents. Sleep. 2012 Oct 1;35(10):1353-8.
Mcneil J, Tremblay MS, Leduc G, Boyer C, Bélanger P,
Leblanc AG, Borghese MM, Chaput JP. Objectively-
measured sleep and its association with adiposity and
physical activity in a sample of Canadian children. J Sleep
Res. 2015 Apr;24(2):131-9.
Meininger JC, Gallagher MR, Eissa MA, Nguyen TQ, Chan
W. Sleep duration and its association with ambulatory
blood pressure in a school-based, diverse sample of
adolescents. Am J Hypertens. 2014 Jul;27(7):948-55.
Meng LP, Liu AL, Hu X, Zhang Q, Du SM, Fang HY, Ma J,
Xu GF, Li Y, Guo HW, Du L, Ma GS. Report on childhood
obesity in China (10): association of sleep duration with
obesity. Biomed Environ Sci. 2012 Apr;25(2):133-40.
Michels N, Verbeiren A, Ahrens W, De Henauw S, Sioen I.
Children's sleep quality: relation with sleep duration and
adiposity. Public Health. 2014 May;128(5):488-90.
Miller AL, Kaciroti N, Lebourgeois MK, Chen YP, Sturza J,
Lumeng JC. Sleep timing moderates the concurrent sleep
duration-body mass index association in low-income
preschool-age children. Acad Pediatr. 2014 Mar-
Apr;14(2):207-13.
Mitchell JA, Rodriguez D, Schmitz KH, Audrain-McGovern J.
Sleep duration and adolescent obesity. Pediatrics. 2013
May;131(5):e1428-34.
Monasta L, Batty GD, Cattaneo A, Lutje V, Ronfani L, Van
Lenthe FJ, Brug J. Early-life determinants of overweight
and obesity: a review of systematic reviews. Obes Rev.
2010 Oct;11(10):695-708.
Moraleda-Cibrián M, O'Brien LM. Sleep duration and body
mass index in children and adolescents with and without
obstructive sleep apnea. Sleep Breath. 2014
Sep;18(3):555-61.
Morley BC, Scully ML, Niven PH, Okely AD, Baur LA, Pratt
IS, Wakefield MA; NaSSDA Study Team. What factors are
associated with excess body weight in Australian
secondary school students? Med J Aust. 2012 Feb
20;196(3):189-92.
Must A, Parisi SM. Sedentary behavior and sleep:
paradoxical effects in association with childhood obesity.
Int J Obes (Lond). 2009 Apr;33 Suppl 1:S82-6.
Nixon GM, Thompson JM, Han DY, Becroft DM, Clark PM,
Robinson E, Waldie KE, Wild CJ, Black PN, Mitchell EA.
Short sleep duration in middle childhood: risk factors and
consequences. Sleep. 2008 Jan;31(1):71-8.
Nugent R, Althouse A, Yaqub Y, Nugent K, Raj R. Modeling
the relation between obesity and sleep parameters in
children referred for dietary weight reduction intervention.
South Med J. 2014 Aug;107(8):473-80.
O'Dea JA, Dibley MJ, Rankin NM. Low sleep and low
socioeconomic status predict high body mass index: a 4-
year longitudinal study of Australian schoolchildren.
Pediatr Obes. 2012 Aug;7(4):295-303.
Ochiai H, Shirasawa T, Shimada N, Ohtsu T, Nishimura R,
Morimoto A, Hoshino H, Tajima N, Kokaze A. Sleep
duration and overweight among elementary
schoolchildren: a population-based study in Japan. Acta
Med Okayama. 2012;66(2):93-9.
Olds T, Blunden S, Dollman J, Maher CA. Day type and the
relationship between weight status and sleep duration in
children and adolescents. Aust N Z J Public Health. 2010
Apr;34(2):165-71.
Olds TS, Maher CA, Matricciani L. Sleep duration or
bedtime? Exploring the relationship between sleep habits
and weight status and activity patterns. Sleep. 2011 Oct
1;34(10):1299-307.
Ozturk A, Mazicioglu M, Poyrazoglu S, Cicek B, Gunay O,
Kurtoglu S. The relationship between sleep duration and
obesity in Turkish children and adolescents. Acta Paediatr.
2009 Apr;98(4):699-702.
Padez C, Mourao I, Moreira P, Rosado V. Long sleep
duration and childhood overweight/obesity and body fat.
Am J Hum Biol. 2009 May-Jun;21(3):371-6.
Park S. The association between short sleep duration and
body mass index among South Korean children and
adolescents. J Sch Nurs. 2013 Apr;29(2):142-50.
Park S. Association between short sleep duration and
obesity among South korean adolescents. West J Nurs
Res. 2011 Mar;33(2):207-23.
Prats-Puig A, Grau-Cabrera P, Riera-Pérez E, Cortés-
Marina R, Fortea E, Soriano-Rodríguez P, de Zegher F,
Ibánez L, Bassols J, López-Bermejo A. Variations in the
obesity genes FTO, TMEM18 and NRXN3 influence the
vulnerability of children to weight gain induced by short
sleep duration. Int J Obes (Lond). 2013 Feb;37(2):182-7.
Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A,
Rogers I, Steer C, Sherriff A; Avon Longitudinal Study of
Parents and Children Study Team. Early life risk factors
for obesity in childhood: cohort study. BMJ. 2005 Jun
11;330(7504):1357.
Reither EN, Krueger PM, Hale L, Reiter EM, Peppard PE.
Ethnic variation in the association between sleep and body
mass among US adolescents. Int J Obes (Lond). 2014
Jul;38(7):944-9.
Rey-López JP, de Carvalho HB, de Moraes AC, Ruiz JR,
Sjöström M, Marcos A, Polito A, Gottrand F, Manios Y,
Kafatos A, Molnar D, Widhalm K, De Henauw S, Moreno
LA; HELENA study. Sleep time and cardiovascular risk
factors in adolescents: the HELENA (Healthy Lifestyle in
Europe by Nutrition in Adolescence) study. Sleep Med.
2014 Jan;15(1):104-10.
Rutters F, Gerver WJ, Nieuwenhuizen AG, Verhoef SP,
Westerterp-Plantenga MS. Sleep duration and body-
weight development during puberty in a Dutch children
cohort. Int J Obes (Lond). 2010 Oct;34(10):1508-14.
Sallinen BJ, Hassan F, Olszewski A, Maupin A, Hoban TF,
Chervin RD, Woolford SJ. Longer weekly sleep duration
predicts greater 3-month BMI reduction among obese
adolescents attending a clinical multidisciplinary weight
management program. Obes Facts. 2013;6(3):239-46.
Sasaki A, Yorifuji T, Iwase T, Komatsu H, Takao S, Doi H. Is
There Any Association between TV Viewing and Obesity
in Preschool Children in Japan? Acta Med Okayama. 2010
Apr;64(2):137-42.
Seegers V, Petit D, Falissard B, Vitaro F, Tremblay RE,
Montplaisir J, Touchette E. Short sleep duration and body
mass index: a prospective longitudinal study in
preadolescence. Am J Epidemiol. 2011 Mar
15;173(6):621-9.
Seicean A, Redline S, Seicean S, Kirchner HL, Gao Y,
Sekine M, Zhu X, Storfer-Isser A. Association between
short sleeping hours and overweight in adolescents:
results from a US Suburban High School survey. Sleep
Breath. 2007 Dec;11(4):285-93.
Sekine M, Yamagami T, Handa K, Saito T, Nanri S,
Kawaminami K, Tokui N, Yoshida K, Kagamimori S. A
dose-response relationship between short sleeping hours
and childhood obesity: results of the Toyama Birth Cohort
Study. Child Care Health Dev. 2002 Mar;28(2):163-70.
Shan XY, Xi B, Cheng H, Hou DQ, Wang Y, Mi J.
Prevalence and behavioral risk factors of overweight and
obesity among children aged 2-18 in Beijing, China. Int J
Pediatr Obes. 2010 Oct;5(5):383-9.
Shi Z, Taylor AW, Gill TK, Tuckerman J, Adams R, Martin J.
Short sleep duration and obesity among Australian
children. BMC Public Health. 2010 Oct 15;10:609.
Shochat T, Cohen-Zion M, Tzischinsky O. Functional
consequences of inadequate sleep in adolescents: a
systematic review. Sleep Med Rev. 2014 Feb;18(1):75-87.
Silva GE, Goodwin JL, Parthasarathy S, Sherrill DL, Vana
KD, Drescher AA, Quan SF. Longitudinal association
between short sleep, body weight, and emotional and
learning problems in Hispanic and Caucasian children.
Sleep. 2011 Sep 1;34(9):1197-205.
Sivertsen B, Pallesen S, Sand L, Hysing M. Sleep and body
mass index in adolescence: results from a large
population-based study of Norwegian adolescents aged
16 to 19 years. BMC Pediatr. 2014 Aug 15;14:204.
Skidmore PM, Howe AS, Polak MA, Wong JE, Lubransky A,
Williams SM, Black KE. Sleep duration and adiposity in
older adolescents from Otago, New Zealand: relationships
differ between boys and girls and are independent of food
choice. Nutr J. 2013 Sep 14;12:128.
Sokolovic N, Kuriyan R, Kurpad AV, Thomas T. Sleep and
birthweight predict visceral adiposity in overweight/obese
children. Pediatr Obes. 2013 Jun;8(3):e41-4.
Spruyt K, Molfese DL, Gozal D. Sleep duration, sleep
regularity, body weight, and metabolic homeostasis in
school-aged children. Pediatrics. 2011 Feb;127(2):e345-
52.
Steele RM, van Sluijs EM, Cassidy A, Griffin SJ, Ekelund U.
Targeting sedentary time or moderate- and vigorous-
intensity activity: independent relations with adiposity in a
population-based sample of 10-y-old British children. Am J
Clin Nutr. 2009 Nov;90(5):1185-92.
Sugimori H, Yoshida K, Izuno T, Miyakawa M, Suka M,
Sekine M, Yamagami T, Kagamimori S. Analysis of factors
that influence body mass index from ages 3 to 6 years: A
study based on the Toyama cohort study. Pediatr Int. 2004
Jun;46(3):302-10.
Sun Y, Sekine M, Kagamimori S. Lifestyle and overweight
among Japanese adolescents: the Toyama Birth Cohort
Study. J Epidemiol. 2009;19(6):303-10.
Sung V, Beebe DW, Vandyke R, Fenchel MC, Crimmins NA,
Kirk S, Hiscock H, Amin R, Wake M. Does sleep duration
predict metabolic risk in obese adolescents attending
tertiary services? A cross-sectional study. Sleep. 2011 Jul
1;34(7):891-8.
Taheri S. The link between short sleep duration and obesity:
we should recommend more sleep to prevent obesity.
Arch Dis Child. 2006 Nov;91(11):881-4.
Tan E, Healey D, Gray AR, Galland BC. Sleep hygiene
intervention for youth aged 10 to 18 years with problematic
sleep: a before-after pilot study. BMC Pediatr. 2012 Dec
7;12:189.
Tatone-Tokuda F, Dubois L, Ramsay T, Girard M, Touchette
E, Petit D, Montplaisir JY. Sex differences in the
association between sleep duration, diet and body mass
index: a birth cohort study. J Sleep Res. 2012
Aug;21(4):448-60.
Taveras EM, Gillman MW, Peña MM, Redline S, Rifas-
Shiman SL. Chronic sleep curtailment and adiposity.
Pediatrics. 2014 Jun;133(6):1013-22.
Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP,
Gillman MW. Short sleep duration in infancy and risk of
childhood overweight. Arch Pediatr Adolesc Med. 2008
Apr;162(4):305-11.
Tian Z, Ye T, Zhang X, Liu E, Wang W, Wang P, Liu G,
Yang X, Hu G, Yu Z. Sleep duration and hyperglycemia
among obese and nonobese children aged 3 to 6 years.
Arch Pediatr Adolesc Med. 2010 Jan;164(1):46-52.
Tikotzky L, DE Marcas G, Har-Toov J, Dollberg S, Bar-Haim
Y, Sadeh A. Sleep and physical growth in infants during
the first 6 months. J Sleep Res. 2010 Mar;19(1 Pt 1):103-
10.
Touchette E, Petit D, Tremblay RE, Boivin M, Falissard B,
Genolini C, Montplaisir JY. Associations between sleep
duration patterns and overweight/obesity at age 6. Sleep.
2008 Nov;31(11):1507-14.
Vaezghasemi M, Lindkvist M, Ivarsson A, Eurenius E.
Overweight and lifestyle among 13-15 year olds: a cross-
sectional study in northern Sweden. Scand J Public
Health. 2012 May;40(3):221-8.
von Kries R, Toschke AM, Wurmser H, Sauerwald T,
Koletzko B. Reduced risk for overweight and obesity in 5-
and 6-y-old children by duration of sleep--a cross-sectional
study. Int J Obes Relat Metab Disord. 2002
May;26(5):710-6.
Wake M, Price A, Clifford S, Ukoumunne OC, Hiscock H.
Does an intervention that improves infant sleep also
improve overweight at age 6? Follow-up of a randomised
trial. Arch Dis Child. 2011 Jun;96(6):526-32.
Weiss A, Xu F, Storfer-Isser A, Thomas A, Ievers-Landis CE,
Redline S. The association of sleep duration with
adolescents' fat and carbohydrate consumption. Sleep.
2010 Sep;33(9):1201-9.
Weiss R, Bremer AA, Lustig RH. What is metabolic
syndrome, and why are children getting it? Ann N Y Acad
Sci. 2013 Apr;1281:123-40.
Wells JC, Hallal PC, Reichert FF, Menezes AM, Araújo CL,
Victora CG. Sleep patterns and television viewing in
relation to obesity and blood pressure: evidence from an
adolescent Brazilian birth cohort. Int J Obes (Lond). 2008
Jul;32(7):1042-9.
Wheaton AG, Perry GS, Chapman DP, Croft JB. Self-
reported sleep duration and weight-control strategies
among U.S. high school students. Sleep. 2013 Aug
1;36(8):1139-45.
Wing YK, Li SX, Li AM, Zhang J, Kong AP. The effect of
weekend and holiday sleep compensation on childhood
overweight and obesity. Pediatrics. 2009
Nov;124(5):e994-e1000.
Wong WW, Ortiz CL, Lathan D, Moore LA, Konzelmann KL,
Adolph AL, Smith EO, Butte NF. Sleep duration of
underserved minority children in a cross-sectional study.
BMC Public Health. 2013 Jul 12;13:648.
Zhu Y, Li AM, Au CT, Kong AP, Zhang J, Wong CK, Chan
JC, Wing YK. Association between sleep architecture and
glucose tolerance in children and adolescents. J Diabetes.
2015 Jan;7(1):10-5.
