
RACE
OF
PHYSICIAN
AND
SATISFACTION
WITH
CARE
AMONG
AFRICAN-
AMERICAN
PATIENTS
Thomas
A.
LaVeist,
PhD,
and
Tamyra
Carroll
Baltimore,
Maryland
The
purpose
of
this
study
is
to
examine
predictors
of
physician-patient
race
concordance
and
the
effect
of
race
concordance
on
patients'
satisfaction
with
their
primary
physicians
among
African
American
patients.
The
specific
research
question
is,
do
African
American
patients
express
greater
satisfaction
with
their
care
when
they
have
an
African
American
physician?
Using
the
Commonwealth
Fund,
Minority
Health
Survey,
we
conduct
multivariate
analysis
of
African
American
respondents
who
have
a
usual
source
of
care
(n
=
745).
More
than
21%
of
African
American
patients
reported
having
an
African
American
physician.
Patient
income
and
having
a
choice
in
the
selection
of
the
physician
were
significant
predictors
of
race
concordance.
And,
patients
who
were
race
concordant
reported
higher
levels
of
satisfaction
with
care
com-
pared
with
African
American
patients
thatwere
not
race
concordant.
(J
NatlMedAssoc.
2002;
94:937-943.)
INTRODUCTION
Race
relations
have
been
among
the
most
vexing
problems
facing
American
culture,
and
healthcare
has
not
been
immune
to
this.
Through
most
of
the
20th
century,
healthcare
facilities
were
racially
segregated,
with
African
Americans
generally
receiving
suboptimal
care.
In
addition,
African
American
physicians
were
typically
barred
from
practicing
medicine
on
white
patients.1
2
While
many
of
these
condi-
tions
have
abated,
vestiges
of
this
history
re-
main.
There
is
substantial
contemporary
evi-
©
2002.
From
the
Center
for
Health
Disparities
Solutions,
Bloomberg
School
of
Public
Health,
Johns
Hopkins
University.
Address
reprint
requests
to
Dr.
Thomas
LaVeist,
Johns
Hopkins
University,
Bloomberg
School
of
Public
Health,
624
North
Broadway,
Baltimore,
MD
21205;
phone
(410)
955-3774;
fax
(410)
614-8964;
or
direct
e-mail
to
dence
of
race
disparities
in
access,
utilization
and
quality
of
care.3"14'15
Among
the
most
commonly
proposed
solu-
tions
to
race
disparities
in
quality
of
care,
is
the
recommendation
to
increase
the
number
of
African
American
healthcare
providers.
This
suggestion
supposes
that
increasing
the
num-
ber
of
providers
will
increase
the
likelihood
that
African
American
patients
will
have
an
African
American
provider.
In
turn,
physician-
patient
race
concordance
is
expected
to
lead
to
better
quality
care
and
greater
patient
satisfac-
tion.28
Medical
schools
have
responded
to
this
proposition
by
increasing
the
production
of
minority
physicians.4'5
Yet,
although
quite
pop-
ular,
the
race
concordance
hypothesis
has
re-
ceived
only
limited
scrutiny.
In
this
paper,
we
address
the
question,
do
African
American
pa-
tients
express
greater
satisfaction
with
their
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
94,
NO.
11,
NOVEMBER
2002
937

DOCTOR
RACE
AND
PATIENT
SATISFACTION
care
when
they
have
an
African
American
phy-
sician?
METHODS
Data
for
this
analysis
came
from
the
1994
Commonwealth
Fund
Minority
Health
Survey
(MHS).
The
MHS
is
a
sample
within
the
con-
tiguous
United
States
of
adults
18
years
of
age
and
older
residing
in
households
with
tele-
phones.6
Interviews
were
conducted
via
tele-
phone
using
random
digit
dialing.
African
Americans
were
over-sampled
in
the
MHS,
re-
sulting
in
a
total
sample
of
1048
African
Amer-
ican
respondents.
The
present
analysis
exam-
ines
the
subsample
of
745 African
American
respondents
who
indicated
that
they
had
a
usual
source
of
care.
Dependent
Variables
The
first
set
of
analyses
examined
predictors
of
race
concordance,
and
the
second
set
exam-
ined
patient
satisfaction.
Race
concordance
was
specified
as
a
binary
variable
indicating
that
the
respondent's
race
is
concordant
with
the
race
of
the
physician.
Patient
satisfaction
is
assessed
by
a
five-item
scale.
Respondents
were
asked
how
good
their
doctor
is
at:
(1)
providing
good
healthcare
overall;
(2)
treating
them
with
dig-
nity;
(3)
making
sure
the
patient
understands
what
he/she
has
been
told;
(4)
listening
to
health
problems;
(5)
being
assessable
by
phone
or
in
person.
The
responses
were
on
a
scale
of
1
to
4,
with
1
being
excellent
and
4
being
poor.
In
the
regression
analysis,
responses
to
the
five
items
were
summarized
to
form
an
index
rang-
ing
from
5
to
20.
This
index
had
a
Chronbach's
Alpha
of
0.81.
Independent
Variables
In
analysis
predicting
race
concordance,
physician
choice
was
the
primary
independent
variable.
Physician
choice
was
measured
by
the
question,
"How
much
choice
you
do
have
in
where
you
go
for
medical
care?"
Respondents
indicating
that
they
have
a
"great
deal"
or
"some"
were
coded
as
having
a
choice,
and
responses
of
"very
little"~
or
"no
choice"
were
coded
as
no
choice.
In
analysis
of
patient
satis-
faction,
physician-patient
race
concordance
was
the
primary
independent
variable.
Covariates
The
covariates
were
sex,
age,
income,
educa-
tion,
and
health
insurance.
Sex
was
specified
as
a
binary
variable
indicating
male.
Age
was
spec-
ified
as
a
set
of
binary
variables
indicating
age:
18-30,
31-40,
41-50,
51-65,
and
66-94.
An-
nual
income
was
specified
as
a
continuous
vari-
able.
Education
was
specified
as
a
set
of
binary
variables
indicating
less
than
high
school
grad-
uate,
some
college,
college
graduate,
and
more
than
college
graduate.
Health
insurance
was
specified
as
a
set
of
binary
variables
indicating
private
insurance,
Medicare,
Medicaid,
and
un-
insured.
RESULTS
Table
1
presents
distributions
of
the
vari-
ables
included
in
the
analysis.
The
table
shows
that
the
respondents
were
evenly
divided
by
gender,
with
50%
of
the
respondents
being
male.
Age
of
the
respondents
was
spread
fairly
evenly
within
a
range
of
18
to
94
years
of
age.
The
median
age
fell
within
the
range
of
be-
tween
41
and
50
years
old.
And
respondents
over
age
66
represented
the
smallest
category
(12.7%).
The
median
income
for
the
sample
was
between
$25,001
and
$35,000
per
annum,
with
91.4%
of
respondents
reporting
a
salary
under
$75,000.
Eighty-two
percent
of
respondents
had
ob-
tained
at
least
a
high
school
education
and
50.8%
received
some
higher
education.
More
than
75%
of
respondents
had
private
health
insurance
and
slightly
less
than
one-fifth
had
Medicare.
Just
over
15%
of
the
respondents
had
Medicaid
and
10%
were
uninsured.
Fi-
nally,
nearly
two-thirds
of
respondents
re-
ported
having
a
choice
for
their
physician.
Table
2
examines
the
distribution
of
physi-
cian's
race
among
African
American
respon-
dents.
The
table
shows
that
nearly
22%
of
re-
spondents
had
an
African
American
doctor.
The
largest
percentage
of
respondents
(58.5%)
938
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
94,
NO.
11,
NOVEMBER
2002

DOCTOR
RACE
AND
PATIENT
SATISFACTION
Table
1.
Sample
Descriptive
Statistics
Variable
Percent
Male
50.0
Age
18-30
20.4
31-40
27.0
41-50
18.9
51-65
20.9
66-94
12.7
Income
<$7,500
13.2
$75,001-$15,000
12.6
$15,001-$25,000
19.3
$25,001-$35,000
1
8.6
$35,001
-$50,000
17.4
$50,001-$75,000
10.3
$75,001-$100,000
5.8
>$
100,000
2.8
Education
<HS
grad
17.7
HS
grad
31.6
Some
college
27.0
College
grad
13.8
Post
college
10.0
Insurance*
Private
75.6
Medicare
19.9
Medicaid
15.4
Uninsured
10.8
Doctor
choice
65.3
*Insurance
status
categories
are
not
mutually
exclusive.
For
example,
a
respondent
can
have
Medicare
and
a
private
healthcare
policy.
Also,
one
could
be
dually
eligible
for
Medicare
and
Medicaid.
reported
having
a
white
physician.
About
10%
of
respondents
had
Asian
or
Pacific
Islander
physicians
and
9.7%
had
a
doctor
who
was
of
Hispanic
descent
or
another
ethnic
group
(His-
panic
physicians
were
not
analyzed
as
a
sepa-
Table
2.
Race
of
Physician
Among
African
American
Respondents
who
Reported
Having
a
Usual
Source
of
Care
Physician's
race
(n=745)
White
436
(58.5%)
Black
162
(21.7%)
Hispanic/other
46
(6.5%)
Asian/pacific
islander
75
(10.1
%)
Table
3.
Logistic
Regression
Analysis
of
Predictors
of
Physician-patient
Race
Concordance,
Odds
Ratio
(95%
Confidence
Interval)
Female
B
Male
.863
(.593,1.25)
Age
18-30
B
31-40
.41
(.24,
.71)
41-50
.47
(.27,
.83)
51-65
.53
(.31,
.92)
66-94
.25
(.11,
.1)
Income
1.13
(1.0,
1.26)
Education
K-12
B
High
School
.62
(.34,
1.13)
Some
College
.73
(.39,
1
.36)
College
Graduate
.64
(.31,
1.30)
Post
College
Degree
.64
(.29,
1.38)
Insurance
Private
B
Medicare
1.43
(.75,
2.74)
Medicaid
.69
(.37,
1.32)
Uninsured
1.19
(.59,
2.39)
Doctor
Choice
1.91
(.1.00,
3.64)
Model
Statistics
Hosmer
and
Lemeshow
X2
=
4.71
df
=
8
p
=
.00
rate
category
because
their
total
numbers
were
too
small,
only
17
respondents
reported
having
a
Hispanic
physician).
Table
3
presents
the
results
of
logistic
regres-
sion
models
examining
predictors
of
race
con-
cordance.
The
table
shows
that
patient's
age,
income,
and
having
a
choice
of
physician
are
significant
predictors
of
physician-patient
race
concordance.
Younger
respondents
were
more
likely
to
be
race
concordant.
Higher
income
was
associated
with
a
greater
likelihood
of
race
concordance.
And,
respondents
who
report
they
have
the
ability
to
choose
their
own
phy-
sician
had
nearly
double
the
odds
of
being
race
concordant
with
their
physician
compared
with
patients
that
did
not
have
choice.
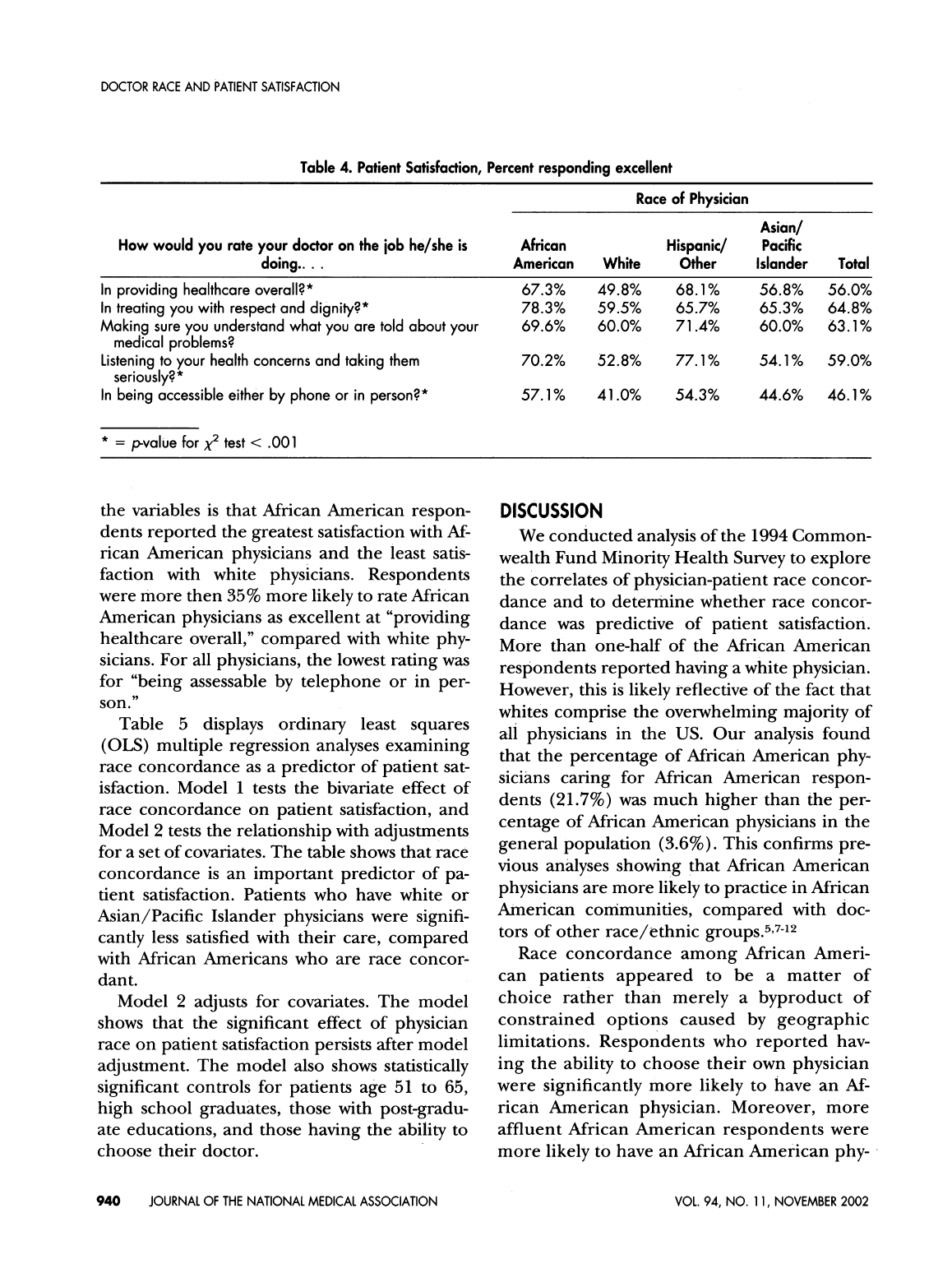
In
Table
4,
the
analysis
turns
to
an
assess-
ment
of
patient
satisfaction.
The
table
displays
bivariate
analysis
of
each
item
comprising
the
five-item
patient
satisfaction
scale
arrayed
by
race
of
physician.
The
general
pattern
among
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
94,
NO.
11,
NOVEMBER
2002
939
DOCTOR
RACE
AND
PATIENT
SATISFACTION
Table
4.
Patient
Satisfaction,
Percent
responding
excellent
Race
of
Physician
Asian/
How
would
you
rate
your
doctor
on
the
job
he/she
is
African
Hispanic/
Pacific
doing....
American
White
Other
Islander
Total
In
providing
healthcare
overall?*
67.3%
49.8%
68.1%
56.8%
56.0%
In
treating
you
with
respect
and
dignity?*
78.3%
59.5%
65.7%
65.3%
64.8%
Making
sure
you
understand
what
you
are
told
about
your
69.6%
60.0% 71.4%
60.0%
63.1%
medical
problems?
Listening
to
your
health
concerns
and
taking
them
70.2%
52.8%
77.1%
54.1%
59.0%
seriously?*
In
being
accessible
either
by
phone
or
in
person?*
57.1%
41.0% 54.3%
44.6%
46.1%
*
=
p-value
for
x2
test
<
.001
the
variables
is
that
African
American
respon-
dents
reported
the
greatest
satisfaction
with
Af-
rican
American
physicians
and
the
least
satis-
faction
with
white
physicians.
Respondents
were
more
then
35%
more
likely
to
rate
African
American
physicians
as
excellent
at
"providing
healthcare
overall,"
compared
with
white
phy-
sicians.
For
all
physicians,
the
lowest
rating
was
for
"being
assessable
by
telephone
or
in
per-
son."
Table
5
displays
ordinary
least
squares
(OLS)
multiple
regression
analyses
examining
race
concordance
as
a
predictor
of
patient
sat-
isfaction.
Model
1
tests
the
bivariate
effect
of
race
concordance
on
patient
satisfaction,
and
Model
2
tests
the
relationship
with
adjustments
for
a
set
of
covariates.
The
table
shows
that
race
concordance
is
an
important
predictor
of
pa-
tient
satisfaction.
Patients
who
have
white
or
Asian/Pacific
Islander
physicians
were
signifi-
cantly
less
satisfied
with
their
care,
compared
with
African
Americans
who
are
race
concor-
dant.
Model
2
adjusts
for
covariates.
The
model
shows
that
the
significant
effect
of
physician
race
on
patient
satisfaction
persists
after
model
adjustment.
The
model
also
shows
statistically
significant
controls
for
patients
age
51
to
65,
high
school
graduates,
those
with
post-gradu-
ate
educations,
and
those
having
the
ability
to
choose
their
doctor.
DISCUSSION
We
conducted
analysis
of
the
1994
Common-
wealth
Fund
Minority
Health
Survey
to
explore
the
correlates
of
physician-patient
race
concor-
dance
and
to
determine
whether
race
concor-
dance
was
predictive
of
patient
satisfaction.
More
than
one-half
of
the
African
American
respondents
reported
having
a
white
physician.
However,
this
is
likely
reflective
of
the
fact
that
whites
comprise
the
overwhelming
majority
of
all
physicians
in
the
US.
Our
analysis
found
that
the
percentage
of
African
American
phy-
sicians
caring
for
African
American
respon-
dents
(21.7%)
was
much
higher
than
the
per-
centage
of
African
American
physicians
in
the
general
population
(3.6%).
This
confirms
pre-
vious
analyses
showing
that
African
American
physicians
are
more
likely
to
practice
in
African
American
communities,
compared
with
doc-
tors
of
other
race/ethnic
groups.5,7-'2
Race
concordance
among
African
Ameri-
can
patients
appeared
to
be
a
matter
of
choice
rather
than
merely
a
byproduct
of
constrained
options
caused
by
geographic
limitations.
Respondents
who
reported
hav-
ing
the
ability
to
choose
their
own
physician
were
significantly
more
likely
to
have
an
Af-
rican
American
physician.
Moreover,
more
affluent
African
American
respondents
were
more
likely
to
have
an
African
American
phy-
940
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
94,
NO.
11,
NOVEMBER
2002

DOCTOR
RACE
AND
PATIENT
SATISFACTION
Table
5.
Ordinary
Least
Squares
(OLS)
Regression
of
Predictors
of
Patient
Satisfaction-race/Ethnic
Specific
Analysis,
Standardized
Coefficient
(P-value)
Model
1
Model
2
Physician
race
Black
White
-.166
(p
=
.0001)
-.55
(p
=
.0002)
Asian/pacific
islander
-.093
(p
=
.02)
-.098
(p
=
.02)
Hispanic/other
.026
(p
=
.53)
.031
(p
=
.44)
Female
B
Male
-
.024
(p
=
.53)
Age
18-30
31-40
.016
(p
=
.75)
4
1-50
.037
(p
=
.45)
51-65
.128(p=
.011)
66-94
.046
(p
=
.44)
Income
.023
(p=
.61)
Education
K-12
High
school
graduate
.115
(p
=
.04)
Some
college
.088
(p
=
.13)
College
graduate
.039
(p
=
.46)
Post
graduate
degree
.131
(p
=
.012)
Insurance
Private
B
Medicare
.045
(p
=
.42)
Medicaid
.001
(p
=
.98)
Uninsured
.059
(p
=
.13)
Patient
does
not
have
ability
to
choose
doctor
B
Patient
has
ability
to
choose
doctor
.169
(p
=
.0001)
Model
statistics
Adj
R2
=
.024
Adj
R2
=
.064
F
=
6.69
F
=
3.83
p
=.000
p
=.000
sician,
compared
with
less
affluent
persons.
These
respondents,
presumably,
have
a
greater
choice
of
providers.
While
physician-patient
race
concordance
leads
to
greater
patient
satisfaction,
there
is
room
for
improvement.
As
Table
4
shows,
Af-
rican
American
respondents
were
more
satis-
fied
with
Hispanic
and
other
race
physicians
at
making
sure
patients
understood
what
they
were
being
told
and
listening
to
patient's
health
concerns
and
taking
them
seriously.
Ad-
ditionally,
only
57.1%
of
respondents
reported
that
African
American
physicians
were
doing
an
excellent
job
at
being
accessible
by
tele-
phone
or
in
person.
We
point
out
that
the
Hispanic/other
physician
category
is
somewhat
of
a
miscellaneous
category,
so
findings
related
to
this
group
must
be
interpreted
with
caution.
However,
it is
meaningful
that
African
Ameri-
can
physicians
did
not
obtain
the
highest
rat-
ings
for
all
categories.
Moreover,
Chen
et
al.,13
demonstrated
that
African
American
physi-
cians
were
as
likely
as
white
physicians
to
fail
to
refer
African
American
cardiac
patients
for
cor-
onary
Angiography
when
the
procedure
was
indicated.
Thus,
while
African
American
pa-
tients
are
more
satisfied
with
their
care,
it
is
not
clear
that
all
dimensions
of
quality
are
en-
hanced
by
race
concordance.
For
example,
are
African
Americans
more
likely
to
receive
pre-
ventive
health
services?
Are
their
health
ser-
vices
utilization
patterns
different?
Is
their
com-
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
94,
NO.
11,
NOVEMBER
2002
941

DOCTOR
RACE
AND
PATIENT
SATISFACTION
pliance
better?
These
questions
remain
to
be
explored
in
future
research.
Nevertheless,
in
spite
of
some
shortcomings
in
satisfaction
among
race
concordant
African
Americans,
our
finding
of
greater
patient
satis-
faction
supports
the
need
for
the
continuation
of
efforts
to
increase
African
American
physi-
cian
production.
One
might
interpret
these
results
as
support-
ing
a
return
to
racial
segregation
in
medicine;
that
is,
that
patients
are
better
off
with
physi-
cians
who
are
of
their
own
racial
or
ethnic
group.
However,
we
would
strenuously
resist
this
interpretation.
Instead,
we
favor
providing
patients
with
an
array
of
options
that
maxi-
mizes
choice,
and
we
view
the
race
of
physician
as
merely
one
factor
to
be
considered
among
many
others.
As
Table
5
shows,
patient
choice
is
also
highly
associated
with
patient
satisfac-
tion.
As
to
the
matter
of
whether
increasing
the
number
of
African
American
physicians
will
lead
to
better
health
outcomes
for
African
Americans,
an
interpretation
of
our
findings
within
the
context
of
other
related
literature
leads
us
to
conclude
that
it
most
likely
will.
Increasing
the
number
of
African
American
physicians
will
expand
the
opportunities
for
African
American
patients
who
choose
to
be
race
concordant.
Our
findings
suggest
that
there
will
be
greater
satisfaction
among
African
Americans
who
are
inclined
to
choose
doctors
in
concordance
with
race.
Previous
findings
demonstrate
that
African
American
physicians
are
more
likely
to
practice
in
minority
and
under-served
communities.7-"1
Studies
of
patient
satisfaction
and
other
related
concepts
(such
as
patient-centeredness)
find
improved
outcomes
in
race
concordant
physi-
cian-patient
pairs.'6
There
is
a
very
limited
lit-
erature
on
race
concordance
and
medical
out-
comes,'3
but
the
one
available
study
indicates
that
African
American
physicians
are
as
likely
as
white
physicians
to
under-refer
African
Ameri-
can
patients
for
heart
surgery.
Chen's'3
find-
ings
are
inconsistent
with
the
findings
in
the
present
analysis,
as
well
as
other
studies,'6"7
and
may
be
anomalous.
Clearly,
there
is
a
need
for
further
study
to
confirm
or
refute
Chen's
findings.
However,
whether
or
not
future
re-
search
confirms
Chen,
patient
satisfaction
is
an
important
outcome
in
its
own
right.
In
addition
to
its
intrinsic
importance
for
individual
health-
care
consumers
and
third-party
payers,
patient
satisfaction
also
is
an
important
determinant
of
health-related
outcomes,
such
as
health
ser-
vices
utilization,'8'19
decision
to
switch
to
an-
other
health
plan,2s23
compliance
with
medical
regimen,24
and
the
decision
to
initiate
malprac-
tice
suits.25
Moreover,
the
Institute
of
Medicine
recommends
including
patient
satisfaction
as
an
indicator
of
quality
of
care.26'27
As
the
African
American
population
contin-
ues
to
grow
and
becomes
increasingly
affluent,
the
demand
for
African
American
physicians
will
grow,
as
well.
However,
as
previous
analyses
have
shown,
the
current
rate
of
African
Amer-
ican
physician
production,
will
not
keep
pace
with
future
demand.5
As
such,
alternatives
such
as
effective
"cultural
competency"
training,
are
needed
if
we
are
to
achieve
the
objective
of
eliminating
race
disparities
in
health,
improve
quality
of
care
among
African
American
pa-
tients,
and
make
the
healthcare
system
respon-
sive
to
the
changing
racial
demographics
of
our
nation.
AKNOWLEDGEMENT
This
research
was
supported
by
a
grant
from
the
Com-
monwealth
Fund
to
Dr.
LaVeist.
REFERENCES
1.
Gamble
VN.
A
legacy
of
distrust:
African
Americans
and
medical
research.
Am
JPrev
Med.
1993;9(6
Suppl):35-38.
2.
Smith
DB.
Health
Care
Divided:
Race
and
Healing
a
Nation.
Ann
Arbor,
MI:
University
of
Michigan
Press,
1999.
3.
Mayberry
RM,
Mili
F,
Ofili
E.
Racial
and
ethnic
differ-
ences
in
access
to
medical
care.
Med
Care
Res
Rev.
2000;57(Suppl
1):108-145.
4.
Carlisle
DM,
Gardner
JE,
Honghu
Liu.
The
entry
of
underrepresented
minority
students
into
US
medical
schools:
an
evaluation
of
recent
trends.
AmJPub
Hlth.
1998;88:1314-1318.
5.
Libby
DL,
Zhou
Z,
Kindig
DA.
Will
minority
physician
supply
meet
US
needs?
Health
Affairs.
1997;16:205-214.
6.
Hogue,
Carol
JR,
Hargraves
MA.
The
Commonwealth
Fund
Minority
Health
Survey
of
1994:
an
overview,
in
Carol
JR,
Hogue,
Hargraves
MA
and
Collins
KS
(eds.),
Minority
health
in
America:
findings
and
policy
implications
from
the
Commonwealth
Fund
942
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
94,
NO.
11,
NOVEMBER
2002

DOCTOR
RACE
AND
PATIENT
SATISFACTION
Minority
Health
Survey,
Baltimore
and
London:
Johns
Hopkins
University
Press,
2000.
7.
Cantor
JC,
Miles
EL,
Baker
LC,
Barker
DC.
Physician
service
to
the
underserved:
implications
for
affirmative
action
in
medical
education.
Inquiry.
1996;33:167-180.
8.
Komaromay
M,
Grumbach
K,
Drake
M,
et
al.
The
role
of
Black
and
Hispanic
physicians
in
providing
health
care
for
un-
derserved
populations.
New
EngJ
Med.
1996;334:1305-1310.
9.
Moy
E,
Bartman
BA.
Physician
race
and
care
of
minority
and
medically
indigent
patients.
JAMA.
1995;273:1515-1520.
10.
Keith
SN,
Bell
RM,
Swanson
AG,
Williams
AP.
Effects
of
affirmative
action
in
medical
schools:
a
study
of
the
class
of
1975.
New
EngJMed.
1985;313:1519-1525.
11.
Lloyd
SM
Jr.,
Johnson
DG.
Practice
patterns
of
Black
physicians:
results
of
a
survey
of
Howard
University
College
of
Medicine
alumni.
J
Nat
Med
Assoc.
1982;74:129
-141.
12.
Rocheleau
B.
Black
physicians
and
ambulatory
care.
Pub
Hlth
Repts.
1978;93:278-282.
13.
Chen
J,
Rathore
SS,
Radford
MJ,
Wang
Y,
Krumholz
HM.
Racial
differences
in
the
use
of
cardiac
catheterization
after
acute
myocardial
infarction.
New
EnglJMed.
2001;344:1443-1449.
14.
Geiger
HJ.
Racial
and
ethnic
disparities
in
diagnosis
and
treatment:
a
review
of
the
evidence
and
a
consideration
of
causes.
In
Unequal
Treatment;
Confronting
Racial
and
Ethnic
Disparities
in
Health
Care.
2002
IOM.
Washington,
DC:
National
Academy
Press.
15.
Kressin
NR,
Peterson
IA.
Racial
differences
in
the
use
of
invasive
cardiovascular
procedures:
review
of
the
literature
and
prescription
for
future
research.
Ann
Intern
Med.
2001;135:352-
366.
16.
Cooper-Patrick
L,
Gallo
Jj,
Gonzales
Jj,
et
al.
Race,
gen-
der,
and
partnership
in
the
patient-physician
relationship.JAMA.
1999;282:583-589.
17.
Saha
S,
Komaromy
MM,
Koepsell
RD,
Bindman
AB.
Patient-physician
racial
concordance
and
the
perceived
quality
and
use
of
health
care.
Arch
Int
Med.
1999;159:997-1004.
18.
Zastoway
TR,
Roghmann
KJ,
Cafferata
GL.
Patient
satis-
faction
and
the
use
of
health
services:
explorations
in
causality.
Med
Care.
1989;27:705-723.
19.
Roghmann
KJ,
Hengst
A,
Zastoway
TR.
Satisfaction
with
medical
care:
its
measurement
and
relation
to
utilization.
Med
Care.
1979;17:461-479.
20.
Murray
BP,
Dwore
RB,
Gustafson
G,
Parsons
RJ,
Vor-
derer
LH.
Enrollee
satisfaction
with
HMOs
and
its
relationship
with
disenrollment.
Managed
Care
Interface.
2000;13:55-61.
21.
Allen
HM
Jr.,
Rogers
WH.
The
consumer
health
plan
value
survey:
round
two.
Hlth
Aff
1998;17:265-268.
22.
Hennelly
VD,
Boxerman
SB.
Disenrollment
from
a
pre-
paid
group
plan:
a
multivariate
analysis.
Med
Care.
1983;21:1154-
1167.
23.
Sorensen
AA,
Wersinger
RP.
Factors
influencing
disen-
rollment
from
an
HMO.
Med
Care.
1981;19:766-773.
24.
Smith
NA,
Ley
P,
Seale
JP,
Shaw
J.
Health
benefits,
satisfaction
and
compliance.
Pat
Educ
Counsel.
1987;10:279-286.
25.
Penchansky
R,
Macnee
C.
Initiation
of
medical
malprac-
tice
suits:
a
conceptualization
and
test.
Med
Care.
1996;34:280-
282.
26.
Hurtado
MP,
Swift
EK,
CorriganJM
(Eds.).
Envisioning
the
National
Health
Care
Quality
Report.
2001
IOM.
Washington
DC:
National
Academy
Press.
27.
Institute
of
Medicine,
Committee
on
Quality
of
Health
Care
in
America.
Crossing
the
Quality
Chasm:
A
New
Health
System
for
the
21st
Century
2001.
IOM.
Washington
DC:
National
Acad-
emy
Press.
28.
LaVeist
TA,
Nuru-Jeter
A.
Is
doctor-patient
race
concor-
dance
associated
with
greater
satisfaction
with
care?
J
Hlth
Soc
Behv.
(forthcoming)
We
Welcome
Your
Comments
Journal
of
the
National
Medical
Association
welcomes
your
Letters
to
the
Editor
about
articles
that
appear
in
the
JNMA
or
issues
relevant
to
minority
health
care.
Address
correspondence
to
Editor-in-Chief,
]NMA,
1012
Tenth
St,
NW,
Washington,
DC
20001;
fax
(202)
371-1162;
or
ktaylor
@nmanet.org.
JOURNAL
OF
THE
NATIONAL
MEDICAL
ASSOCIATION
VOL.
94,
NO.
1
1,
NOVEMBER
2002
943
