
Page 1
DISTRICT OF COLUMBIA
Department of Health Care Finance (DHCF)
Supplemental Form for Long Term Care Benefits
Instructions
This is a supplemental form for those who would like to apply for Medicaid assistance to pay for Long-Term Care
services and supports to include assistance with paying for a nursing home or intermediate care facility for the
Developmentally Disabled (ICF/DD) and the Home and Community-Based Services (HCBS) Waiver Programs.
The HCBS Waiver Program includes:
•
Persons Who Are Elderly or Physically Disabled (EPD),
•
Persons with Intellectual and/or Developmental Disabilities (IDD) and
•
Individual and Family Support (IFS).
Program Overview
The Elderly and Individuals with Physical Disabilities (EPD) Waiver Program
Institutional Transition status provides a range of services for individuals receiving care in a nursing facility who are
transitioning to the community to receive services under the EPD Waiver Program. It is limited to the transition period
before discharge form the nursing facility.
Institutional Transition
The EPD Waiver program provides a range of services to assist adults age 65 and older and individuals with physical
disabilities to live as independently as possible in their homes and communities. These services are provided in
addition to other services offered through DC Medicaid.
Intellectual and Developmental Disabilities (IDD) Waiver Program
The IDD Waiver provides a range of services for individuals with intellectual or developmental disabilities who want to
live as independently as possible in their homes or communities. These services are provided, according to a person’s
need, in addition to other services offered by DC Medicaid.
Institutional Care Program (Nursing Facility and ICF/IDD Facility)
The Institutional Care Program provides coverage to people receiving institutionalized level of care in a nursing
facility or in an Intermediate Care Facility for the developmentally disabled.
Individuals may not be eligible for the Institutional Care Program or the Waiver Programs because they transferred
assets for less than fair market value within 60 months (5 year) look-back period. They may be eligible for other
Medicaid services.
If you want to apply for EPD services, you must first contact the DC Office of Aging and Disabilities Resource Center
(ADRC)
at (202) 724-5626, Monday thru Friday from 8:00 A.M. to 5:00 P.M. If you want to apply for IDD, you must
contact the
Department of Disability Services (DDS) Intake & Eligibility Office at (202) 730-1745, Monday thru Friday
from 8:00 A.M. to
5:00 P.M.
You or someone you have chosen to act on your behalf will need to complete and submit this supplemental form.

Page 2
When filling out this supplemental form, please be sure to:
•
Answer all the questions and fill out all the sections correctly and completely.
•
Sign and date the application
•
Send proof of all documentation that applies to you. Please review, “Checklist of Needed Documentation for
your Long-Term Care/Waiver”
If you are not applying for EPD services or IDD, you can:
1.
Mail this application to:
Long-Term Care
Unit 645 H Street, NE
5th Floor
Washington, DC 20002
2. You can also bring this supplemental form to the 645 H Street, NE Service Center.
3. You can email this application to esanursing.hom[email protected]ov
4. You can also fax this application to (202) 724-8963
If you are applying for EPD services or IDD, you will submit your application to ADRC or DDS and they will submit the
complete application package to the Economic Security Administration on your behalf.
Important Notice:
All Long-Term Care applicants are required to submit a complete application. If you are applying for EPD Waiver, a
complete application must include:
•
A completed and signed Supplemental Form for Long Term Care Benefits (This form)
•
A completed and approved Level of Care by DHCF or its agent
Once all the information above is provided, the application is considered complete. The Aging and Disability Resource
Center (ADRC) will then submit your complete application to the Economic Security Administration (ESA) for
processing. Once ADRC submits the complete application, to ESA, ESA will make an eligibility determination within 45
calendar days.
If you are applying for the
IDD Waiver
, a complete application must include:
•
A completed and signed Supplemental Form for Long Term Care Benefits (This form)
•
A completed Level of Care Form
If you are applying for Medicaid coverage in a
Nursing Facility or ICF/DD facility
, a complete application must include:
•
A completed and signed Supplemental Form for Long Term Care Benefits (This form)
•
A completed and signed Start of Care Form
•
For nursing facility, a completed and approved Level of Care by DHCF or its agent
•
Please Note: For ICF/IDD facility, a completed and approved Level of Care
Please note that the clinician (Doctor or APRN) that completes your Level of Care Form MUST be a Medicaid provider.
If the clinician who completes your Level of Care is not an enrolled Medicaid provider, they MUST complete a
Provider Application. Your clinician may contact the Provider Enrollment Unit at (202) 698-2000 or download a
streamlined application at: https://www.dc-medicaid.com/dcwebal/documenInformation/getDocument/14934
To find a clinician who is a Medicaid Provider, please visit our website at: www.dc-medicaid.com and click “Search for
Provider” on the left hand corner.
Your application will be submitted for processing when all the required documents, including the LOC Form are received.
Please note that your application for the EPD Waiver, the IDD Waiver, Nursing facility coverage or coverage in an ICF/
DD facility must be complete with the documents described above. If the application is not signed and complete and
the required signed documents are not provided with the application to ESA, the application will not be registered and
processed. ESA Will only begin processing the application when all of the required documents are signed, completed,
and submitted to ESA.
The information you give us on this application is kept confidential as required by the Federal and District law.

Page 3
Service Center Locations
What
program(s) would you like to apply for
?
Institutional Care Home and Community-Based Waiver
Nursing Facility or Skilled Nursing Facility
Intermediate Care Facilities for Persons with
Intellectual and Developmental Disabilities (ICF/
IDD)
Elderly and Individuals with Physical Disabilities
(EPD)
Intellectual and Developmental Disabilities (IDD)
Money Follows the Person
Individual and Family Support (IFS)
Anacostia Service Center
2100 Martin Luther King Jr. Ave.,
SE Washington, DC 20020
Fax: (202) 727-3527
Congress Heights Service Center
4049 South Capitol St.,
SW Washington, DC 20032
Fax: (202) 645-4524
Taylor Street Service Center
1207 Taylor St., NW
Washington, DC
20011
Fax: (202) 576-8740
Fort Davis Service Center
3851 Alabama Ave., SE
Washington, DC
20020
Fax: (202) 645-6205
H Street Service Center
645 H St., NE
Washington, DC 20002
Fax: (202) 724-8964
Customers may call the ESA
Call Center at (202) 727-5355
to learn which Service Center
serves their address

Page 4
Language Access Support
If you speak another language, you have the right to free language assistance services. Call (202) 727-5355 or TTY/TDD
711 (855) 532-5465. District law requires that agencies provide you with information and assistance in your language
for free. If you do not receive help in your language, please call the DC Office of Human Rights at (202) 727-4559 and
press 0.
ATENCIÓN: si habla español, tiene a su disposición servi-
Dè ɖɛ nìà kɛ dyéɖé gbo: Ɔ jǔ ké m
̀
[Ɓàsɔ
́
ɔ
̀
-wùɖù-po-nyɔ
̀
] jǔ
ní, nìí, à wuɖu kà kò ɖò po-poɔ
̀
ɓɛ
́
ìn m
̀
gbo kpáa. Ɖá (202)
727-5355 (TTY/TDD 711 (855) 532-5465).
Ige nti: O buru na asu Ibo asusu, enyemaka diri gi site na
call (202) 727-5355 (TTY/TDD 711 (855) 532-5465).
AKIYESI: Ti o ba nso ede Yoruba ofe ni iranlowo lori ede wa
fun yin o. E pe ero ibanisoro yi (202) 727-5355 (TTY/TDD
711 (855) 532-5465).
, ,
-
(202) 727-
5355 (TTY/TDD 711 (855) 532-5465)
注意事項:日本語を話される場合、無料の言語支援をご利用いただけ
ます。(202) 727-5355(TTY/TDD 711 (855) 532-5465)
まで、お電話にてご連絡ください。
주의: 한국어를 사용하시는 경우, 언어 지원 서비스를 무
료로 이용하실 수 있습니다. (202) 727-5355 (TTY/TDD
711 (855) 532-5465)번으로 전화해 주십시오.
(202)
727-5355
(TTY/TDD
711
(855)
532-
5465).
ACHTUNG: Wenn Sie Deutsch sprechen, stehen Ihnen
kostenlos sprachliche Hilfsdienstleistungen zur Verfügung.
Rufnummer: (202) 727-5355 (TTY/TDD 711 (855) 532-
5465).
cios gratuitos de asistencia lingüística. Llame al (202) 727-
5355 (TTY/TDD 711 (855) 532-5465).
ማስታወሻ: የሚናገሩት ቋንቋ ኣማርኛ ከሆነ የትርጉም እርዳታ ድርጅቶች፣ በነጻ
ሊያግዝዎት ተዘጋጀተዋል ወደ ሚከተለው ቁጥር ይደውሉ (202) 727-5355
(መስማት ለተሳናቸው: TTY/TDD 711 (855) 532-5465).
注意:如果您使用繁體中文,您可以免費獲得語言援助服
務。請致電(202) 727-5355 (TTY/TDD 711 (855) 532-5465
ATTENTION : Si vous parlez français, des services d’aide
linguistique vous sont proposés gratuitement. Appelez le
(202) 727-5355 (ATS : TTY/TDD 711 (855) 532-5465).
PAUNAWA: Kung nagsasalita ka ng Tagalog, maaari kang
gumamit ng mga serbisyo ng tulong sa wika nang walang
bayad. Tumawag sa (202) 727-5355 (TTY/TDD 711 (855)
532-5465).
ВНИМАНИЕ: Если вы говорите на русском языке, то вам
доступны бесплатные услуги перевода. Звоните (202)
727-5355 (TTY/TDD 711 (855) 532-5465).
ATENÇÃO: Se fala português, encontram-se disponíveis
serviços linguísticos, grátis. Ligue para (202) 727-5355
(TTY/TDD 711 (855) 532-5465).
ATTENZIONE: In caso la lingua parlata sia l’italiano, sono
disponibili servizi di assistenza linguistica gratuiti. Chiamare
il numero (202) 727-5355 (TTY/TDD 711 (855) 532-5465).
CHÚ Ý: Nếu bạn nói Tiếng Việt, có các dịch vụ hỗ trợ ngôn
ngữ miễn phí dành cho bạn. Gọi số (202) 727-5355 (TTY/
TDD 711 (855) 532-5465.
What is the Language that
you need to read?
English
Spanish
Vietnamese
French
Korean
Amharic
Chinese
(Mandarin
)
Chinese
(Cantonese
)
Other
What Language do you
need to speak to get ESA
services?
English
Spanish
Vietnamese
French
Korean
Amharic
Chinese
(Mandarin
)
Chinese
(Cantonese
)
Other
If you need an interpreter,
what language do you need
interpreted?
English
Spanish
Vietnamese
French
Korean
Amharic
Chinese
(Mandarin
)
Chinese
(Cantonese
)
Other

Page 5
Do you want free language interpretation?
Yes (a case worker will assist you) No (complete and sign waiver below)
I,
, acknowledge that The Department of Human Services (DHS) has notified
me
of my right to a professional and trained interpreter as required by the D.C. Language Access Act of 2004 at no
cost to me. By signing below, I agree that I have refused this service and opted to rely on interpreter assistance by
someone I have identified. I am aware that this individual was not identified by or vetted through DHS and that DHS
is neither responsible for the provision of these services nor does DHS incur any liability that may result from these
services. I am also aware that this waiver only applies to this one instance. If I require interpreter assistance from
DHS in the future, I will notify the agency directly to request this service.
Sign here Date
Applicant or Representative Signature
OFFICE USE: This statement was orally translated into (language) by (name) ,
who is a language line interpreter, professional in person interpreter, or multilingual DHS employee because a written
translation was not available in that language or the customer was unable to read in his/her spoken language.

Page 6
SECTION 1
Personal
Information
Name
Date of Birth
Sex
Male
Female
Social Security Number
Current Address or your address prior to entering the
Long Term Care Facility:
Do you plan on returning to this residence upon
discharge?
Yes No
Name and Address of the Long Term Care Facility:
Date you entered Facility:
SECTION 2
Information on Spouse
(Complete this information even if you are not applying for your spouse)
Name
Date of Birth
Address
Social Security Number
SECTION 2A
Please list any dependent children, dependent parents, and dependent
siblings that live in your home.
Last name
First name
Middle
Sex
Date of
Social
Relation
Do you
Gross
Initial
Birth
Security
to You
claim this
Monthly
Number
person
Income
(SSN)
as a
dependent
on you tax
return?

Page 7
SECTION 3
Legal Representation
(Do you have one of the following acting on your behalf? Please answer)
Yes No
If you checked “
yes
” please provide the following information.
Conservator
Yes No
Name
Address
Do you pay a monthly Conservator fee?
Yes No
If yes, the Fee Amount:
Telephone Number
Representative Payee
Yes No
Name
Address
Do you pay a monthly Rep. Payee fee?
Yes No
If yes, the Fee Amount:
Telephone Number
Authorized Representative
Yes No
First Name
Address
Last Name
Telephone Number

Page 8
SECTION 4
Income of Applicant and/or Spouse
Please tell us about any income or benefits that you and your spouse are currently receiving, have applied for, or
have been denied. If you or your spouse check an income type below, please provide more information about the
income type(s) in the table below.
Supplemental Security Income (SSI)
Social Security Disability Income (SSDI)
Social Security Retirement Income
Alimony
Worker’s Compensation
Unemployment Benefits
Business Income
Rental Income
Lump Sum Payment
Black Lung Benefits
Veteran’s Pension/Benefits
Pension or Retirement
Disability/Sick
Civil Service
Union Benefits
Other (describe):
Type of Benefit/Income
Receiving
Income or
Benefits
Persons
Receiving
Income or
Benefits
Amount
Application
Status
If applied,
Application or
Denial Date
Yes
No
Self
Spouse
$
Receiving
Applied For
Denied
Yes
No
Self
Spouse
$
Receiving
Applied For
Denied
Yes
No
Self
Spouse
$
Receiving
Applied For
Denied
Yes
No
Self
Spouse
$
Receiving
Applied For
Denied

Page 9
SECTION 5
Assets Currently Owned by You and Your Spouse
Please provide the value(s) of all assets owned by you and your spouse below. If you or your spouse own any assets
below, please attach proof when you submit this form. If you or your spouse do not currently own any assets, you
can skip this section.
Asset Type
Name of Owner(s)
Fair Market Value
Amount Owed
Date Acquired
Bank or Credit Union
Account
$
$
Stocks/Bonds/Mutual
Funds
$
$
Certificates of Deposit
$
$
Annuity/Trust Funds/Trust
Accounts
$
$
2nd Bank or Credit Union
Account
$
$
Your Home
$
$
Vacation Home
Address:
$
$
Land
Address:
$
$
Other Real Property
Type:
Address:
$
$
Boats/Recreational
Vehicles/Motor Homes
Type
$
$
Cash-Including Cash
Surrender Value of any
Life Insurance Policies
$
$
NOTE: If you need additional space to provide additional addresses for the property that you or your spouse own,
please attach a separate sheet of paper.

Page 10
SECTION 6
Assets when you entered the Long Term Care Facility
Married Individuals ONLY:
You or your spouse can request a resource assessment at the beginning of your first continuous period of stay in a facility.
Resource assessment is completed to determine how much of a married couple’s total resources may be protected
or set aside for the spouse in the community, and how much, if any should count towards the spouse who needs
care in a
facility setting or home and community-based services program. This protection is called “Spousal Impoverishment’,
which recognizes the importance of protecting a portion of a married couple’s total resources to account for the needs
of the spouse who remains in the community. Completing Section 6 below will help you to protect the maximum
amount of your resources under the law
If you have a spouse who lived with you before you entered the Long Term Care Facility, you need to list below the
amount of assets you or your spouse had when you entered the facility. You can skip this section if this situation
does not apply to you.
Asset Type
Name of Owner(s)
Fair Market Value
Amount Owed
Date Acquired
Bank or Credit Union
Account
$
$
Stocks / Bonds / Mutual
Funds
$
$
Certificates of Deposit
$
$
Annuity / Trust Funds /
Trust Accounts
$
$
2nd Bank or Credit Union
Account
$
$
Your Home
$
$
Vacation Home (Please
provide address below)
$
$
Land (Please provide
address below)
$
$
Boats/Recreational
Vehicles/Motor Homes
Type
$
$
Cash-Including Cash
Surrender Value of any
Life Insurance Policies
$
$
If you own any property, which is different from your current address, please list the addresses below:
Address 1:
Address 2:
Address 3:
Address 4:
NOTE: If you need additional space to provide additional addresses for the property that you or your spouse own,
please attach a separate sheet of paper.

Page 11
SECTION 7
Transfer of Assets
(Have you or your spouse given away or transferred anything of value in the last five years?
This would include money in bank accounts, stocks, bonds, real estate or other possessions
of value, or creation of an annuity.)
Yes No
If
yes
, complete the following:
Date of
Transfer
Who transferred
the asset?
Who received
the transferred
asset?
Description of
Asset
Value of Asset
at Transfer
Amount
received for
Asset
$
$
Date of
Transfer
Who transferred
the asset?
Who received
the transferred
asset?
Description of
Asset
Value of Asset
at Transfer
Amount
received for
Asset
$
$
Date of
Transfer
Who transferred
the asset?
Who received
the transferred
asset?
Description of
Asset
Value of Asset
at Transfer
Amount
received for
Asset
$
$
Date of
Transfer
Who transferred
the asset?
Who received
the transferred
asset?
Description of
Asset
Value of Asset
at Transfer
Amount
received for
Asset
$
$
Date of
Transfer
Who transferred
the asset?
Who received
the transferred
asset?
Description of
Asset
Value of Asset
at Transfer
Amount
received for
Asset
$
$
Attach another page if you transferred additional assets

Page 12
Additional Questions to See How Much You May Need To Pay for Your Care
Do you own or rent a home?
Yes No
Do you expect to return to this home within six (6) months?
Yes No
If you expect to return, will your spouse or any of your dependents continue to stay in your home?
Yes No
If your home will be unoccupied, you may qualify for a Home Maintenance Allowance that will reduce the amount you
have to pay for your Long-Term Care costs. If your home will be occupied by your spouse, his/her Spousal Allowance
may be increased because of high shelter expenses. Please list the amount you pay for the following:
Rent/Mortgage $
Real Estate Taxes $
Home Insurance $
Home Association Fees $
Condo/Co-Op Maintenance Fees $
SECTION 8
Health Insurance Information
Medicare Information
(from your Medicare Card)
Do you have Medicare?
Yes No
Type of Coverage
Part A
Part B
Medicare Claim Number
Effective Date
Part A
Part B
Does your spouse have
Medicare?
Yes No
Type of Coverage
Part A
Part B
Medicare Claim Number
Effective Date
Part A
Part B
Other Health Insurance
Do you have other health insurance?
Yes No
Amount of Monthly Premium
$
Does your spouse have other health insurance?
Yes No
Amount of Monthly Premium
$
If you or your spouse have other health insurance, including a Medicare supplement policy, please complete the boxes
below and attach a copy (front and back) of the insurance cards.
Health Insurance
Company - Name and
Address
Monthly Premium
Policy Number
Type of Coverage
(Medigap, Retiree,
RX, etc.)
Self
Spouse

Page 13
SECTION 9
Information on Past Medical Bills/Expenses
If you have medical bills for services that you received before the month of this application, we may be able to help you
pay some or all those bills.
If you don’t want us to pay those bills, or Medicaid rules do not allow us to pay the bills, we may be able to reduce
what you will need to pay for your long term care services.
You can ask for Medicaid to cover your medical bills for up to three months prior to the month of this application. We
call this the retroactive period. For District of Columbia (DC) Medicaid to pay for those months, you must have met the
Medicaid eligibility requirements during those months and incurred expenses that would have been covered by
Medicaid. If you
are eligible for the retroactive period, we will reimburse you for the bills you already paid for those months.
Retroactive Medicaid may cover prior Skilled Nursing Facility, Nursing Facility, and Intermediate Care Facilities for
Individuals with Intellectual Disabilities expenses but may not cover other long-term care services.
If you do not want retroactive benefits, you can ask us to use your unpaid medical bills to help you qualify for Long-
Term Care/Home and Community-Based Services (LTC/HCBS) if you are over the income limit or to reduce the
amount that you will need to pay for your long term care services for this month and future months if you meet the
LTC/HCBS income limits. You can use any unpaid medical bills no matter how old they are. This includes unpaid bills
for long-term care services. If you want us to apply your past bills to your future long-term care costs, then you will
still be responsible for paying those past bills.
If your income is over the Long-Term Care /Home and Community-Based Services (LTC/HCBS) income limit, you
may still
be able to get LTC/HCBS Services by showing that you have high medical expenses. This is called Medicaid
“Spend down.”
To get Medicaid under Spend down, you must have a certain amount of medical bills. The total amount
of medical bills you need is your “deductible.” When you have enough bills, including some past bills, you will meet
your deductible and you may be eligible under Spend down. Medicaid will not pay the bills you count towards your
deductible. After you meet your
deductible, Medicaid may pay for some or all of your other medical bills. If you are
over-income for LTC/HCBS services, you
can use past medical bills to meet your Spend down deductible.
Under Spend down rules for LTC, you can also qualify based on the projected Medicaid reimbursement rate cost of
the institutional care you expect to receive during a six month Spend down period. If we approve LTC based on the
projected Medicaid reimbursement rate costs, you are still responsible for paying these projected costs. If we use your
projected LTC costs to Spend down to Medicaid, you can still use your past medical bills to reduce the remaining
amount you will need to pay for your LTC. You can use paid and unpaid bills from the current and past three months for
Spend down. You can also use unpaid bills that are more than three months old and old bills that were just paid
during the past three months. If you are found to be over-income and need to use Spend down to get LTC/HCBS
services, we will send you a notice telling you the amount of your deductible. If you provide bills with your application
that you ask us to use for Spend down for LTC/ HCBS services, we will send you an additional notice saying how
much you still owe. We will use the projected Medicaid reimbursement rate cost of institutional care towards your
Spend down. You can also provide any other bills you want to use.
If a third party insurance, like Medicare or other health insurance paid or is responsible for paying your medical bill,
we cannot use the bill to reduce the amount you will need to pay for your LTC/HCBS services. For more information,
visit your local ESA Service center or call the DC Department of Human Services Call Center at (202) 727-5355.
Page 14
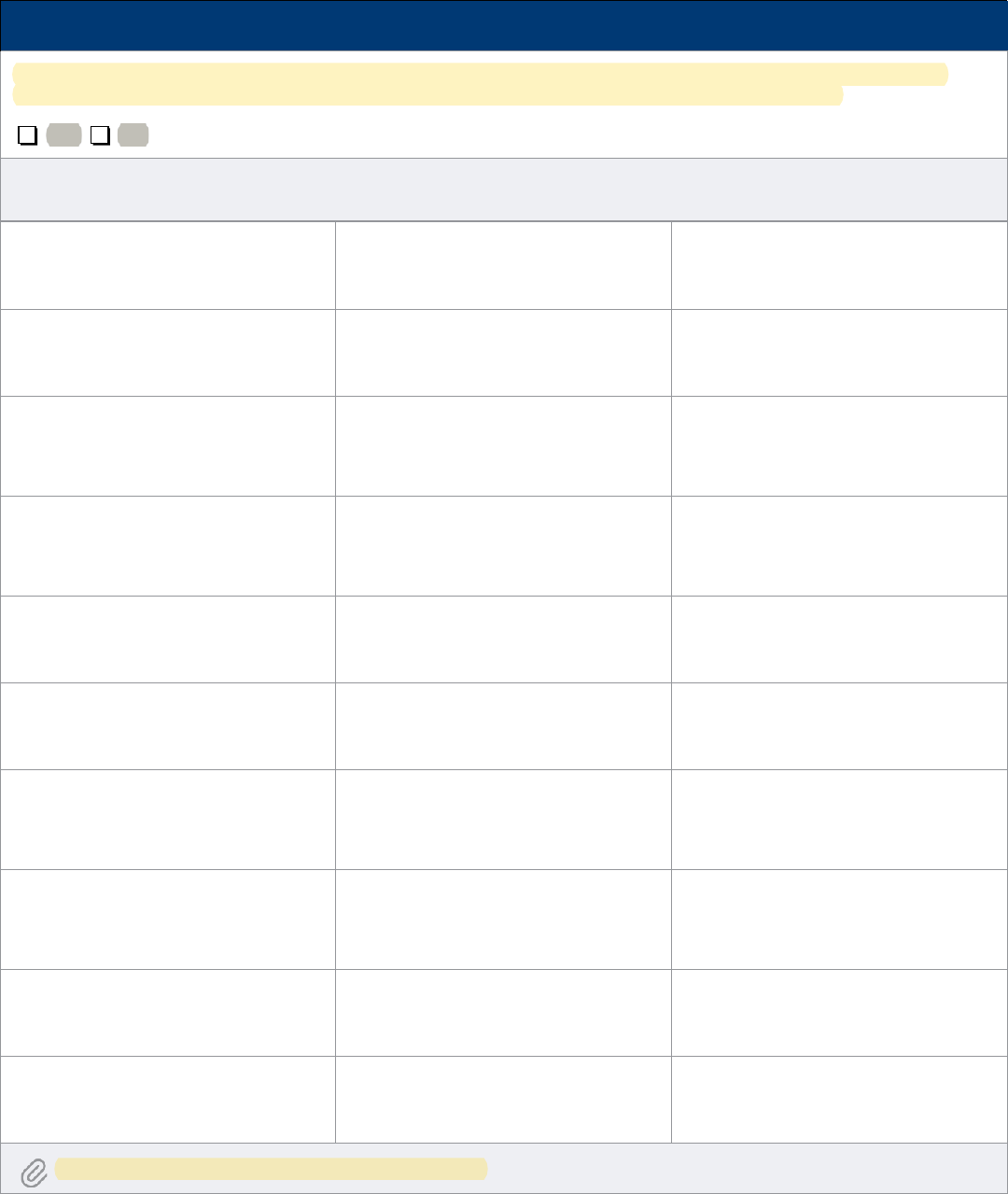
SECTION 9
Listing of Past Medical Expenses
Do you have any past paid or unpaid medical bills, not being used to determine retroactive Medicaid coverage?
(examples include Nursing Home expenses, Prescription drugs, Dental bills, Home Health Care costs, etc.)
Yes No
If you answered “
yes
” to the above question, list the type and amount of these past medical bills that may be used to
determine eligibility and/or to calculate your share of the monthly costs for care in a Long Term Facility.
Type of Medical Service
Date of Medical Service
Amount Billed for Medical Service
Type of Medical Service
Date of Medical Service
Amount Billed for Medical Service
Type of Medical Service
Date of Medical Service
Amount Billed for Medical Service
Type of Medical Service
Date of Medical Service
Amount Billed for Medical Service
Type of Medical Service
Date of Medical Service
Amount Billed for Medical Service
Type of Medical Service
Date of Medical Service
Amount Billed for Medical Service
Type of Medical Service
Date of Medical Service
Amount Billed for Medical Service
Type of Medical Service
Date of Medical Service
Amount Billed for Medical Service
Type of Medical Service
Date of Medical Service
Amount Billed for Medical Service
Type of Medical Service
Date of Medical Service
Amount Billed for Medical Service
Attach another page if you have additional medial expenses

Page 15
SECTION 9
Listing of Past Medical Expenses
•
By signing below, I give my permission to DHS to get information about me and my spouse. DHS can get this
information from those officials or institutions that have knowledge of my situation. I give all of these parties my
permission to give information about me to DHS. I have reviewed the information in my application, and I believe
that all of the information on this entire application is true and correct. I know if I give false information, I may be
breaking the law and I could be at risk of criminal prosecution and penalties. I know that state and federal officials
will check this information. I agree to help and cooperate with their potential investigations.
•
By signing below, I understand that the District may seek recovery for all the bills paid by Medicaid on my
behalf, including nursing home, waiver, or services provided in other medical institutions.
•
By signing below, I have reviewed my Rights and Responsibilities attached to this Supplemental Form. I understand my
responsibilities and agree to cooperate as required.
•
By signing below, I understand that if I, or my spouse, purchased an annuity on or after February 8, 2006, and I
receive long term care services, the District of Columbia must be named a remainder beneficiary of the annuity by
virtue of the provision of medical assistance relating to long-term care services.
•
Authorized Representative(s): If the applicant cannot sign this form, you may sign it for them. By signing, you certify
that this person wants to apply for benefits and agrees to the conditions above.
Nursing Facility and Intermediate Care Facility Applicants/Beneficiaries Only
By signing below, I understand that if I am determined ineligible for Medicaid Long Term Care Services due to excess
income and placed on a spend-down, the nursing facility or intermediate care facility may use the projected Medicaid
reimbursement rate for medical institution expenses to help me meet my spend-down. If the projected medical
expenses are used to meet my spend-down amount and I am determined eligible for Medicaid long term care
coverage, I understand that I am still responsible for paying the medical institution the projected medical institution
expenses.
Signature Date
Representative Signature Date

Page 16
Appendix A
Notice of Rights and Responsibilities
General Rules
You must give true and complete information. If you lie or give false information, you may lose your benefits. You could also
be
fined and go to prison. We may verify your information to make sure it is correct. We may check on your income, your
Social Security information, and your immigration information. We verify this information through computer matching
programs. We may also interview you and do a home visit.
You may designate someone as your authorized representative. This gives them the authority to file the application on
your behalf. If you designate someone to be your authorized representative, the agency will send them copies of notices
that they
send to you. They may submit verifications on your behalf as well.
Your case may be chosen for a Quality Control review. This is a detailed review of all of your information. It may
include
some personal interviews and a review of your medical records. By applying, you agree to cooperate with the
state or federal reviewers. If you refuse to cooperate, you may lose all or part of your benefits. If you are under
investigation or are fleeing to
avoid the law, we may share your information with federal and local agencies.
Under federal and District law, you must provide your Social Security Number (if you have one) if you are seeking Medicaid.
(See 42 CFR 435.910) Your SSN will be used to verify your identity, prevent receipt of duplicate benefits, and make required
program changes. The Department of Human Services (DHS) computer system uses your SSN to verify your income by using
records from the Internal Revenue Service, the Social Security Administration, and the DC Child Support Services Division
(CSSD).
Medical Assistance Rules
After your complete application is submitted to ESA, you will get a decision about your Medical Assistance within 45 days
(or 60 days if DHS must determine if you are disabled). If you do not get a notice within this period, please call the DC
Medicaid
Branch on (202) 698-4220 or the Change Center on (202) 727-5355.
Out of Pocket Reimbursement Information:
If you paid for drug prescriptions, doctor visits, or hospitalizations during a time that you were eligible for Medicaid, you may
be able to be reimbursed for the expenses.
REQUIREMENTS: You may be eligible for reimbursement if during a period of time you or a family member were eligible for
Medicaid and
a.
You paid for drug prescriptions, doctor visits, or hospitalizations; or
b.
You are still paying a bill or are being asked to pay a bill by a pharmacy, clinic, doctor, or hospital for drug
prescriptions,
doctor visits, or hospitalizations.
If you believe that you are entitled to reimbursement, you must request reimbursement within six (6) months of the date
you
went to the pharmacy, clinic, doctor, or hospital, or within six (6) months of the date you learned you were eligible for
Medicaid,
whichever is later.
You must complete and submit a Medicaid Reimbursement Request Form to the DC Department of Health Care
Finance. You can get a copy of the form at any ESA office, or you can download a copy at https://www.dc-
medicaid.com/dcwebportal/ nonsecure/recipientForms.
IF YOU HAVE QUESTIONS OR IF YOU NEED HELP COMPLETING THE FORM OR OBTAINING REQUESTED INFORMATION
CONTACT:
a.
The Medicaid Recipient Claims Research Team of the D.C. Department of Health Care Finance (DHCF) at (202) 698-2009.
b.
Terris Pravlik & Millian, LLP, 1816 12th Street NW, Suite 303, Washington, DC 20009, (202) 682-0578, who will
provide you with free legal assistance.

Page 17
A DECISION ON YOUR REIMBURSEMENT CLAIM MUST BE MADE WITHIN 90 DAYS:
a.
The Medicaid Recipient Claims Research Team must make a decision on your reimbursement claim within 90 days
from the time you file your claim. If no decision is made within those 90 days, your claim will be treated as valid, and
you will be
paid within 15 days after the end of the 90 day period.
b.
If you are not satisfied with the decision of the Medicaid Recipient Claims Research team, you have a right to a
fair
hearing. You may request a fair hearing by calling the Office of Administrative Hearings at (202) 442-9094. The
Office of Administrative Hearings is located at 441 4th Street, NW; Washington, DC 20001-2714.
c.
If you are not satisfied with the result of the fair hearing, you may appeal to the DC Court of Appeals within 30 days.
You may be able to obtain free legal assistance to help you present your case at the hearing or on appeal. If you are a
member of the class certified by the court in Salazar v. District of Columbia, Civil Action No. 93-452 (TSC) (D.D.C.), you may
contact Terris, Pravlik & Millian, LLP at 1816 12th Street, NW, Suite 303 Washington, DC 20009 or (202) 682-0578.
Free legal assistance for beneficiaries who are not members of the Salazar class may be available from the following
organizations:
Bread for the City Legal Clinic, (202) 480-8950 or (202) 791-3982 Legal Aid Society, (202) 628-1161
Legal Counsel for the Elderly, (202) 434-2120
Neighborhood Legal Services, (202) 832-6577
University Legal Services, (202) 547-4747
Estate Recovery
The District may seek recovery for all the bills paid by Medicaid on your behalf, including nursing home, waiver or services
provided in other medical institutions. For more information on estate recovery, contact the Department of Health
Care
Finance, Health Operations Administration, Third Party Liability Division at (202) 698-2000.
Lawsuits
If you sue or enter into settlement negotiations with a third party for a medical claim or injury, you must provide written
notice of the action (either by personal service or certified mail) within 20 calendar days to the Medical Assistance
Administration,
Third Party Liability Section, 441 4th Street, NW, Suite 1000-South, Washington, DC 20001. If you have
questions, call (202) 698-
2000.
Reporting Changes
You must report changes in your income, Medicare status, marital or institutional status, who lives with you, or if you
move
from D.C. You may want to report a change of District address, changes in your shelter costs and changes in medical
expenses. To report a change, call (202) 727-5355. You must call us by the 10th day of the month after the change. You may
also call the LTC unit at (202) 698-4220 to report changes that will affect what you need to pay for your Long-Term Care
services.
Confidentiality
By applying, you give DHS permission to talk with your employer, your landlord, your nursing facility, your bank, your
doctor,
and other people who have information about you. You also give these people your permission to give
information about
you to DHS. In addition, you also give DHS permission to look at your motor vehicle records, wage
data, tax information, and other government records. DHS keeps all of your information confidential. DHS does not
release your records without your
permission, except as permitted or required by law.

Page 18
Discrimination is Against the Law
DHCF and DHS comply with applicable Federal civil rights laws and do not discriminate on the basis of race, color, national
origin, age, disability, or sex. DHCF and DHS do not exclude people or treat them differently because of race, color,
national
origin, age, disability, or sex.
The Department of Healthcare Finance (DHCF) and the Department of Human Services (DHS):
•
Provide free aids and services to people with disabilities to communicate effectively with us, such as:
-
Qualified sign language interpreters
-
Written information in other formats (large print, audio, accessible electronic formats, other formats)
•
Provide free language services to people whose primary language is not English, such as:
-
Qualified interpreters
-
Information written in other languages
If you need these services, contact Ms. Surobhi Rooney at (202) 442-5916.
If you believe that the either DHCF or DHS has failed to provide these services or discriminated in another way on the
basis of
race, color, national origin, age, disability, or sex, you can file a grievance with:
Ms. Surobhi Rooney, DHCF Civil Rights Coordinator 441 4th Street, NW
Washington DC, 20001
Phone: (202) 442-5916
Email: [email protected]
You can file a grievance in person or by mail, fax, or email. If you need help filing a grievance, Ms. Surobhi Rooney is available
to
help you.
You can also file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights
electronically through the Office for Civil Rights Complaint Portal, available at
https://ocrportal.hhs.gov/ocr/portal/lobby. jsf, or by phone 1-800- 368-1019 or mail at: U.S. Department of Health and
Human Services 200 Independence Avenue, SW Washington, DC 20201
Fair Hearings
If you think that DHS has made a mistake, then you can get a Fair Hearing. Call 202-698-4650 to find out more. You can also call
(202) 727-8280. At a Fair Hearing, you can ask someone else to speak for you. This could be an attorney, a friend, a relative,
or someone else. You can also bring witnesses. We will pay for transportation to the Fair Hearing for you and your witnesses.
We may also pay for some of your other costs. You can also get free legal help for a Fair Hearing. Call one of the agencies
below to
talk to a lawyer or counselor.
Free Legal Help
Neighborhood Legal Services
680 Rhode Island Avenue, NE (202) 832-6577
4609 Polk Street, NE (Ward 7) (202) 832-6577
2811 Pennsylvania Avenue, SE (Ward 8) (202) 832-
6577
Legal Counsel for the Elderly (60 years or older)
601 E Street, NW (202) 434-2120
Legal Aid Society 666 11th Street, NW Suite 800 (202) 628-1161
Terris Pravlik & Millian, LLP
1816 12th Street NW, Suite 303, Washington, DC
20009 (202) 682-0578
