
NHPCO Facts and Figures
2021 EDITION
Published October 2021

NHPCO Facts and Figures | 2021 EDITION rganization
Table of Contents
Please see the Data Sources Section
at the end of this report for details
on the data sources used within this
publication.
Section 1: Introduction
z About this report
z What is hospice care?
z How is hospice care delivered?
z What services are provided?
z Location of Care
z Levels of Care
z Volunteer Services
z Bereavement Services
Section 2: Who Receives
Hospice Care
z How many Medicare beneiciaries
who died in 2019 received care?
z What proportion of Medicare
decedents were served by hospice?
z What % of Medicare Advantage
decedents were enrolled in hospice
between 2015 and 2019?
z What are the characteristics of
Medicare beneiciaries who received
hospice care?
• Gender
• Age
• Race
• Principal Diagnosis
Section 3: How Much Care
was Received
z Length of Stay
z Days of Care
z Discharges and Transfers
z Location of Care
Section 4: How Does Medicare
Pay for Hospice
z Medicare spending
z Percent of Days by Spending
z Percent of Days by Level of Care
Section 5: Who Provides Care
z How many hospices were in
operation in 2019
z Tax Status
Reference: Data Sources
and Methodology
Suggested Citation
1

NHPCO Facts and Figures | 2021 EDITION rganization
Section 1: Introduction
About this Report
NHPCO Facts and Figures provides an annual overview of hospice care
delivery. This overview provides speciic information on:
z Hospice patient characteristics
z Location and level of care
z Medicare hospice spending
z Hospice provider characteristics
z Volunteer and bereavement services
Currently, most hospice patients have their costs covered by Medicare,
through the Medicare Hospice Beneit. The indings in this report
relect those patients who received care in 2019 provided by hospices
certiied by the Centers for Medicare and Medicaid Services (CMS) and
reimbursed under the Medicare Hospice Beneit.
What is hospice care?
Considered the model for quality compassionate care for people facing a
life-limiting illness, hospice provides expert medical care, pain management,
and emotional and spiritual support expressly tailored to the patient’s
needs and wishes. Support is provided to the patient’s family as well.
Hospice focuses on caring, not curing. In most cases, care is provided in
the patient’s private residence, but may also be provided in freestanding
hospice facilities, hospitals, nursing homes, or other long-term care facili-
ties. Hospice services are available to patients with any terminal illness.
Hospices promote inclusiveness in the community by ensuring that all
people regardless of race, ethnicity, color, religion, gender, disability, sex-
ual orientation, age, disease, or other characteristics have access to the
hospice’s programs and services.
2

NHPCO Facts and Figures | 2021 EDITION rganization
Introduction (continued)
How is hospice care delivered?
Typically, a family member serves as the primary caregiver for the patient and, when
appropriate, helps make decisions for the terminally ill individual. Members of the hospice
staff make regular visits to assess the patient and provide additional care or other
services. Hospice staff is on-call 24 hours a day, seven days a week.
The hospice team develops a care plan that meets each patient’s individual needs for pain
management and symptom control. This interdisciplinary team, as illustrated in Figure 1,
usually consists of the patient’s personal physician; hospice physician or medical director;
nurses; hospice aides; social workers; bereavement counselors; clergy or other spiritual
counselors; trained volunteers; and speech, physical, and occupational therapists, if needed.
What services are provided?
The interdisciplinary hospice team:
z Manages the patient’s pain and other symptoms;
z Assists the patient and family members with the emotional, psychosocial, and spiritual aspects of dying;
z Provides medications and medical equipment;
z Instructs the family on how to care for the patient;
z Provides grief support and counseling;
z Makes short-term inpatient care available when pain or symptoms become too dificult to manage at home,
or when the caregiver needs respite time;
z Delivers special services like speech language pathology and physical therapy when needed;
z Provides grief support and counseling to surviving family and friends.
Location of Care
The majority of hospice care is provided in the place the patient calls home. In addition to private residences, this includes
nursing homes and residential facilities. Hospice care may also be provided in freestanding hospice facilities and hospitals
(see Levels of Care).
&
3

NHPCO Facts and Figures | 2021 EDITION rganization
Introduction (continued)
Levels of Care
Hospice patients may require differing intensities of care during the course of their illness.
While hospice patients may be admitted at any level of care, changes in their status may require
a change in their level of care.
The Medicare Hospice Beneit affords patients four levels of care to meet their clinical needs:
Routine Home Care, Continuous Home Care, Inpatient Respite Care, and General Inpatient Care.
Payment for each covers all aspects of the patient’s care related to the terminal illness, including
all services delivered by the interdisciplinary team, medication, medical equipment, and supplies.
z Routine Hospice Care (RHC) is the most common level of hospice care. With this type of care,
an individual has elected to receive hospice care at their residence.
z Continuous Home Care (CHC) is care provided for between 8 and 24 hours a day to manage
pain and other acute medical symptoms. CHC services must be predominately nursing
care, supplemented with caregiver and hospice aide services and are intended to maintain the
terminally ill patient at home during a pain or symptom crisis.
z Inpatient Respite Care (IRC) is available to provide temporary relief to the patient’s primary
caregiver. Respite care can be provided in a hospital, hospice facility, or a long-term care facility
that has suficient 24-hour nursing personnel present.
z General Inpatient Care (GIP) is provided for pain control or other acute symptom management
that cannot feasibly be provided in any other setting. GIP begins when other efforts to manage
symptoms are not suficient. GIP can be provided in a Medicare certiied hospital, hospice
inpatient facility, or nursing facility that has a registered nursing available 24 hours a day to
provide direct patient care.
4

NHPCO Facts and Figures | 2021 EDITION rganization
Introduction (continued)
Volunteer Services
The U.S. hospice movement was founded by volunteers who continue
to play an important and valuable role in hospice care and operations.
Moreover, hospice is unique in that it is the only provider with Medicare
Conditions of Participation (CoPs) requiring volunteers to provide at
least 5% of total patient care hours.
Hospice volunteers provide service in three general areas:
z Spending time with patients and families (“direct support”)
z Providing clerical and other services that support patient care and
clinical services (“clinical support”)
z Engaging in a variety of activities such as fundraising, outreach and
education, and serving on a board of directors (“general support”).
Bereavement Services
Counseling or grief support for the patient and loved ones is an essential
part of hospice care. After the patient’s death, bereavement support is
offered to families for at least one year. These services can take a variety
of forms, including visits, written materials about grieving, phone or vid-
eo calls, and support groups. Individual counseling may be offered by the
hospice or the hospice may make a referral to a community resource.
Some hospices also provide bereavement services to the community
at large, in addition to supporting patients and their families.
See page 24 for details on methodology and data sources, including cited
references within the report.
5
NHPCO Facts and Figures | 2021 EDITION rganization
Section 2: Who Receives Hospice Care
How many Medicare beneiciaries received hospice care in 2019?
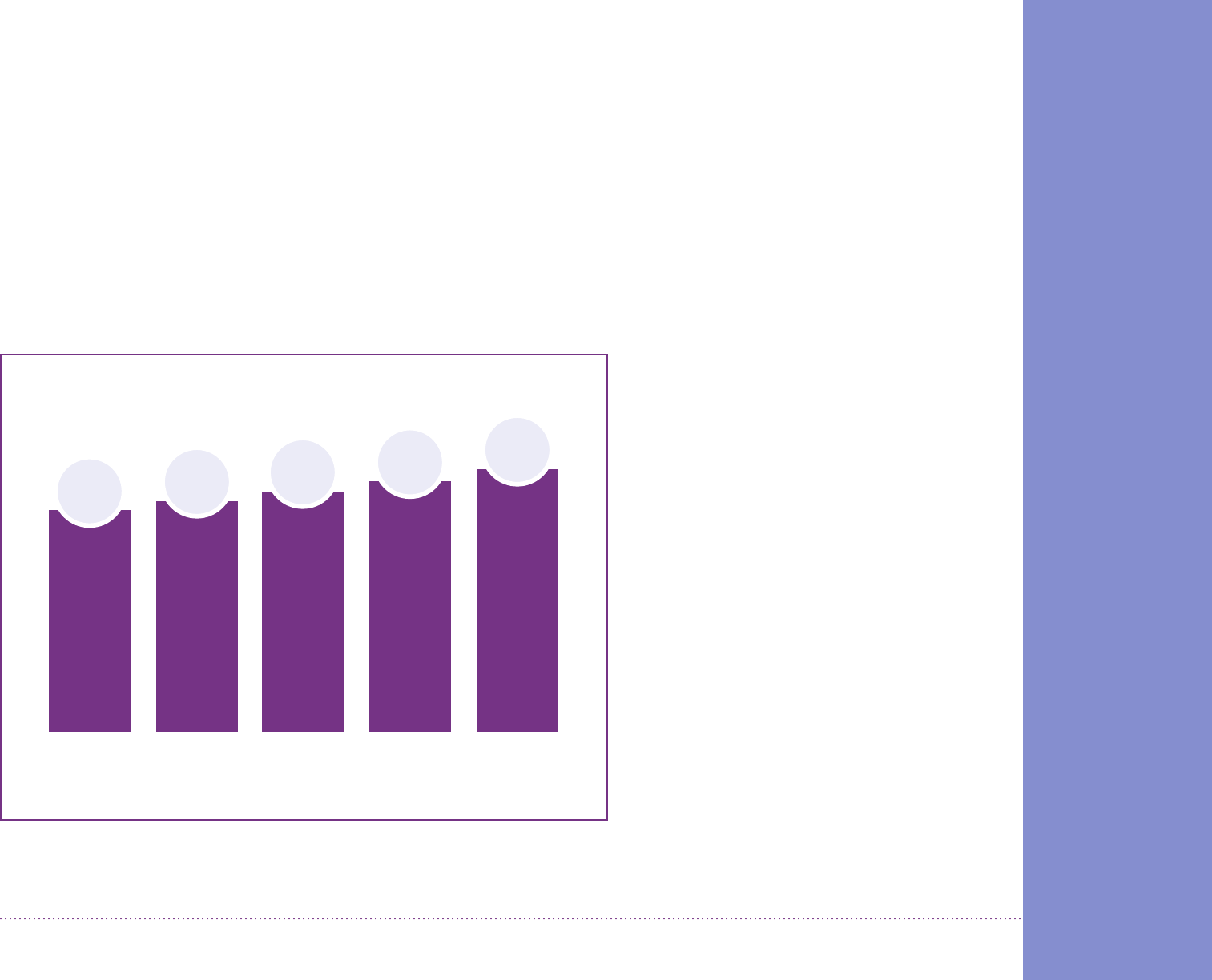
As seen in Figure 1, 1.61 million Medicare beneiciaries who died were enrolled in hospice care for one day or more in 2019.
This is a 3.9 percent increase from 2018. This includes patients who:
z Died while enrolled in hospice
z Were enrolled in hospice in 2018 and continued to receive care in 2019
z Left hospice care alive during 2019 (live discharges)
2015 2016 2017 2018 2019
1.49M
1.43M
1.38M
Figure 1: Medicare Beneiciaries
1.55M
6
Source: MedPAC March Report to Congress, Table 11-3, Various years
*Includes all states, Washington, D.C., U.S. territories, and other
1.61M

NHPCO Facts and Figures | 2021 EDITION rganization
Who Receives Hospice Care (continued)
What % of Medicare Advantage
Decedents Enrolled in Hospice
between 2015 and 2019?
As demonstrated in Figure 3, utilization of
the hospice beneit remains a bit higher
among decedents enrolled in Medicare
Advantage (MA) plans than among
Traditional Medicare users, while the
trendline for hospice usage continues to
increase in both groups. MA decedents
who utilized the hospice beneit rose from
51.1 percent in 2015 to 53.2 percent in 2019.
During the same period, Traditional
Medicare decedents utilizing the hospice
beneit rose from 47.6 percent in 2015 to
50.7 percent in 2019.
What proportion of Medicare
decedents were served by
hospice in 2019?
Of all Medicare decedents in 2019, as seen
in Figure 2, 51.6 percent received one day or
more of hospice care and were enrolled in
hospice at the time of death.
Medicare Advantage Beneiciaries Traditional Medicare Beneiciaries
Figure 3: Growth of Medicare Advantage Hospice Patients
2015
48.6%
2016
49.7%
2018
50.6%
7
Source: MedPAC March 2021 Report to Congress, Table 11-2 and
MedPAC March 2018 Report to Congress, Table 12-3
Source: MedPAC March 2021 Report to Congress, Table 11-2 and MedPAC March 2018 Report
to Congress, Table 12-3
2017
49.8%
2019
51.6%
54
53
52
51
50
49
48
47
2015 2016 2017 2018 2019
51.1
%
51.9
%
51.6
%
52.3
%
53.2
%
47.6
%
48.7
%
48.9
%
49.7
%
50.7
%
Figure 2: Percent of Medicare Decedents Receiving
1 or more Days of Hospice Care in 2019

NHPCO Facts and Figures | 2021 EDITION rganization
Who Receives Hospice Care (continued)
What are the characteristics of Medicare beneiciaries who received hospice care in 2019?
Figure 4: Patient Gender
In 2019, among beneiciaries who
identiied as female and died in 2019,
56.2% used hospice and 43.8% did not.
Among beneiciaries who identiied
as male and died in 2019, 46.7% used
hospice and 53.3% did not.
Patient Age
In 2019, as shown in Figure 5, nearly 63 percent of Medicare
decedents age 85 years and older utilized the Medicare hospice
beneit, while progressively smaller percentages of decedents in
younger age groups received hospice care. Figure 6 shows that two of
the four Medicare beneiciary age groups identiied by MedPAC in its
March 2021 Report to Congress saw increased usage of the Medicare
hospice beneit over the ive year period from 2015 to 2019.
56.2%
used hospice
46.7%
used hospice
62.7%
52.2%
41.0%
29.4%
<65
65-74
75-84
85 and older
Figure 5: % of Patients by Age group for 2019
9
Source: MedPAC March 2021 Report to Congress, Table 11-2.
Figure 6: % Change over 5 Years
2015 2016 2017 2018 2019
25
30
35
40
45
50
55
60
65
29.9
%
41.2
%
49.5
%
57.1
%
30.1
%
41.5
%
50.7
%
59.2
%
28.3
%
40.3
%
50.5
%
59.7
%
28.8
%
40.6
%
51.2
%
61.1
%
29.4
%
41.0
%
52.2
%
62.7
%
■ <65 ■ 65-74 ■ 75-84 ■ 85=<
Source: MedPAC March 2021 Report to Congress, Table 11-2.
Among Medicare decedents
who identiied as male
Among Medicare decedents
who identiied as female

NHPCO Facts and Figures | 2021 EDITION rganization
Who Receives Hospice Care (continued)
What are the characteristics of Medicare beneiciaries who received hospice care in 2019?
Patient Race
In 2019, almost 54 percent of White Medicare decedent beneiciaries used the Medicare hospice beneit (53.8 percent). Nearly
43 percent (42.7) of Hispanic Medicare beneiciaries and almost 41 percent (40.8) of Black Medicare beneiciaries enrolled
in hospice in 2019. More than 38 percent of Asian American and American Indian/Alaska Native Medicare decedents used
hospice in 2019.
Figure 7: % of Medicare decedents by race who used hospice
10
Source: MedPAC March 2021 Report to Congress, Table 11-2
Note: In previous years, the NHPCO Facts and Figures has presented data on the share of Medicare beneiciaries
who used hospice by race. In an effort to focus on equity, we are now presenting data from the 2019 MedPAC
March report to Congress, Table 11-2, focused on the percentage of Medicare decedents by race who used hospice.
100%
100%
100%
100%
100%
White 53.8%
Hispanic 42.7%
Black 40.8%
Asian American 39.8%
American Indian/Alaska Native 38.5%
Hospice utilization by race Medicare decedents by race

NHPCO Facts and Figures | 2021 EDITION rganization
What are the
characteristics of
Medicare beneiciaries
who received hospice
care in 2019?
Principal Diagnosis
The principal hospice
diagnosis is the diagnosis
that has been determined to
be the most contributory to
the patient’s terminal
prognosis. Speciic
diagnoses have been
collapsed into major disease
groupings in Figures 8 and 9
to the right. 2019 showed
that more Medicare hospice
patients had a principal
diagnosis of Alzheimer’s/
Dementia/Parkinson’s than
any other disease.
Principal diagnosis categories
of Stroke, Respiratory, and
Circulatory/Heart have
grown the most since 2014.
Who Receives Hospice Care (continued)
11
* In 2002, 2007 and 2013, severe malnutrition includes debility unspeciied and adult failure to thrive. Those diagnoses were disallowed and no longer used in later years.
Source: CMS-1675-P, FY 2018 Hospice Wage Index and Payment Rate Update and Hospice Quality Reporting Requirements and CMS-1754-P Medicare Program; FY 2022 Hospice
Wage Index and Payment Rate Update, Hospice Conditions of Participation Updates, Hospice and Home Health Quality Reporting Program Requirements
Figure 9: Number of Medicare Decedents Using Hospice by Top 15 Diagnoses
200,000
250,000
300,000
350,000
400,000
150,000
100,000
50,000
0
Alzheimers, Dementias,
Parkinsons
Circulatory/Heart Cancer Respiratory Kidney DiseaseStroke/CVA *Severe Malnutrition
■
FY 2002
■
FY 2007
■
FY 2013
■
FY 2016
■
FY 2019
■
FY 2002
■
FY 2007
■
FY 2013
■
FY 2016
■
FY 2019
Figure 8: Percentage of Medicare Decedents Using Hospice by Top 15 Principal Diagnoses
Alzheimers, Dementias,
Parkinsons
Circulatory/Heart Cancer Respiratory Kidney DiseaseStroke/CVA *Severe Malnutrition
0
5
10
15
20
25
22%
16%
12%
8%
4.9%
1%
1.6%
9%
15%
14%
1.3%
9%
9%
10%
9%
6.4%
4%
3%
2% 2%
5.4%
9%
12%
16%
19%
20.9%
5%
6% 6%
7%
7.1 %
56,180
56,283
152,605
35,197
26,897
55,303
219,788
133,085
160,226
82,184
34,459
198,537
113,564
100,006
167,580
60,815
31,800
148,453
284,618
139,603
124,256
106,982
27,629
22,261
336,419
156,693
78,579
113,259
62,760
20,741
24,467

NHPCO Facts and Figures | 2021 EDITION rganization
Section 3: How Much Care Is Received?
Year
Total Days
(in millions)
Average Length
of Stay
Median Length
of Stay
Number of
Patients (in
millions)
2015 95.9 86.7 17 days 1.38
2016 101.2 87.8 18 days 1.42
2017 106.3 89.3 18 days 1.49
2018 113.5 90.3 18 days 1.55
2019 121.8 92.6 18 days 1.61
Length of Stay
The average Length of Stay (LOS) for Medicare patients enrolled in hospice in 2019 was 92.6 days. The median length of stay
(MLOS) was 18 days.
Source: MedPAC March 2021 Report to Congress, Table 11-3 and the MedPAC March 2018 Report to Congress, Table 12-4
Table 1: Average and Median Length of Stay
12

NHPCO Facts and Figures | 2021 EDITION rganization
How Much Care Is Received (continued)
Days of Care by Length of Stay in 2019
z 10% of patients were enrolled in hospice for 2 days or less.
z 25% of patients were enrolled in hospice for 5 days or less.
z 50% of patients were enrolled for 18 days or less.
z 75% of patients were enrolled for 85 days or less.
z At the 90th percentile, 10% of patients were enrolled for more than 266 days.
Figure 10: Days of Care
10th percentile 2 days or less
25th percentile 5 days or less
50th percentile 18 days or less
75th percentile 85 days or less
90th percentile 266 days or less
Source: MedPAC March 2021 Report to Congress, Figure 11-1.
13

NHPCO Facts and Figures | 2021 EDITION rganization
How Much Care Is Received? (continued)
14
Figure 11: Days of Care by Principal Diagnosis for 2019
180160140120100806040200
All
Heart (CHF and Other
Heart Disease)
Cancers
CVA/Stroke
Chronic Kidney Disease/
Kidney Failure
Lung (COPD and
Pneumonias)
Other
Alzheimer’s, Dementia,
and Parkinson’s
■ Average Lifetime Length of Stay ■ Median Lifetime Length of Stay ■ Average Length of Stay
Days of Care
Figure 11 depicts the average lifetime, average and median lifetime length of stay for major hospice disease categories. Average
and median lifetime lengths of stay are deined by CMS as “the sum of all days of hospice care across all hospice elections.” In
2019, as seen in Figure 11, patients with Alzheimer’s, dementias and Parkinson’s used the Medicare Hospice beneit for the
greatest average, lifetime average, and median length of stay in days. This contrasts with chronic kidney disease/kidney failure
and cancer patients, who utilized the Medicare hospice beneit for a much lower average and median number of days in 2019.
Source: FY 2022 Hospice Wage Index and Quality Reporting Proposed Rule, Table 6
Note: Lifetime length of stay is calculated for decedents who were using hospice at the time of death or before death and relects the total number of days the
decedent was enrolled in the Medicare hospice beneit during his or her lifetime.
98.9
44.3
53.5
82.1
107.6
108
148.3
169
20
8
17
14
24
20
34
52
77.3
35.6
45.7
64.2
85.4
82.2
114.7
126.9

NHPCO Facts and Figures | 2021 EDITION rganization
How Much Care Is Received? (continued)
*Calculations are based on total number of discharges which includes patients who were dis-
charged more than one time in 2019.
Table 2: Discharge by Type and Reported Reason, 2017-2019
Reason for Discharge 2017 2018 2019
All discharges 16.7% 17.0% 17.4%
Patient-Initiated Live Discharges
Revocation 6.4 6.6 6.5
Transferred to another hospice 2.1 2.2 2.3
Hospice-Initiated Live Discharges
No longer terminally ill 6.5 6.3 6.5
Moved out of service area 1.4 1.6 1.7
Discharged for cause 0.3 0.3 0.3
16
Source: MedPAC March 2021 Report to Congress, Table 11-11.
Live Discharges and Transfers
In 2019, out of all Medicare hospice discharges, 17.4 percent of all Medicare beneiciaries using hospice were discharged alive,
with patient-initiated and hospice-initiated discharges being about equal.

NHPCO Facts and Figures | 2021 EDITION rganization
How Much Care Is Received? (continued)
Figure 12: Average Days by Location of Care
Figure 13: Median Days by Location of Care
17
Source: MedPAC March 2021 Report to Congress, Table 11-4
Location of Care
In 2019, most of days of care were provided
at a private residence followed by nursing
facilities and assisted living facilities.
Average days by location of care as shown in
Figure 12 were 95 days at a private residence,
109 days in nursing facilities, and 161 days in
assisted living facilities. Median length of
stay by location of care, shown in Figure 13,
were 27 days at a private residence, 22 days
in nursing facilities and 56 days in assisted
living facilities.
Average Median
Private Residence 95 27
Nursing Facility 109 22
Assisted Living Facility 161 56
Table 3: Location of Care by
Average and Median Days of
Care for 2019
0
10
20
30
40
50
60
2015 2016 2017 2018 2019
■ Private Residence ■ Nursing Facility ■ Assisted Living Facility
0
20
40
60
80
100
120
140
160
180
2015 2016 2017 2018 2019
■ Private Residence ■ Nursing Facility ■ Assisted Living Facility
105
20
20
20
21
22
106
105
106
109
89
26
26 26 26 27
90
91 93
95
152
51 51 51
54
56
152 153
155
161

NHPCO Facts and Figures | 2021 EDITION rganization
Section 4: How Does Medicare Pay
for Hospice?
Medicare paid hospice providers a total of $20.9 billion dollars for care provided in 2019, representing
an increase of 8.5% over the previous year.
2015
$15.9B$15.9B
2017
$17.9B$17.9B
2016
$16.8B$16.8B
2018
$19.2B$19.2B
Figure 14: Medicare Spending
18
$20.9B$20.9B
2019
Source: MedPAC March 2021 Report to Congress, Table 11-3 and MedPAC March 2018 Report to Congress,
Table 12-4.

NHPCO Facts and Figures | 2021 EDITION rganization
How Does Medicare Pay for Hospice? (continued)
Spending by Level of Care
In 2019, the vast majority of Medicare spending for hospice
care was for care at the routine home care (RHC) level.
Table 4: Percent of Days by Spending
Table 5: Percent of Days by Level of Care
Level of Care (LOC) 2019
Routine Home Care (RHC) 93.8%
General Inpatient Care (GIP) 4.9%
Inpatient Respite Care (IRC) 0.3%
Continuous Home Care (CHC) 0.9%
19
Source: FY 22 Hospice Wage Index, Proposed Rule, Table 5
Level of Care (LOC) 2015 2016 2017 2018 2019
Routine Home Care (RHC) 97.9% 98.0% 98.0% 98.2% 98.3%
Continuous Home Care (CHC) 0.3% 0.3% 0.2% 0.2% 0.2%
Inpatient Respite Care (IRC) 0.3% 0.3% 0.3% 0.3% 0.3%
General Inpatient Care (GIP) 1.6% 1.6% 1.3% 1.2% 1.2%
Source: MedPAC March Report to Congress, various years and FY 2022 Hospice Wage
Index and Quality Reporting Proposed Rule, April 2021

NHPCO Facts and Figures | 2021 EDITION rganization
Section 5: Who Provides Care?
How many hospices were in operation in 2019?
Over the course of 2019, there were 4,840 Medicare certiied hospices in operation based on claims
data. This represents an increase of 18.3% since 2014.
20152014 20172016 2018
4,199
4,092
4,488
4,382
4,639
Figure 15: Number of Operating Hospices
20
4,840
18.318.3
%%
2019
MedPAC March 2021 Report to Congress, Table 11-1. and MedPAC March 2018 Report to Congress, Table 12-3.

NHPCO Facts and Figures | 2021 EDITION rganization
Who Provides Care? (continued)
Tax Status
As shown in Figure 19, the growth in hospice ownership is being driven by the growth in for-proit ownership. As
reported by MedPAC in the March 2021 Report to Congress, between 2018 and 2019, the number of for-proit hospices
increased by 6.3 percent, while the number of nonproit hospices increased by 0.2 percent, and government owned
hospices declined by 5.7 percent. As of 2019, about 71 percent of hospices were for proit, 26 percent were nonproit,
and 3 percent were government owned.
Figure 16: Providers by Type
21
Source: MedPAC March Report to Congress, Various Years
0
1000
2000
3000
4000
5000
6000
2015 2016 2017 2018 2019
■ For-proit ■ Nonproit ■ Government

NHPCO Facts and Figures | 2021 EDITION rganization
Data Sources
The data sources primarily used for this report are from the
Medicare Payment Advisory Commission (MedPAC) March
Report to Congress (various years) and the FY 2022
Hospice Wage Index and Quality Reporting Proposed Rule,
published in the Federal Register on April 14, 2021. See cited
sources through out the report for each table and igure.
For data references provided by MedPAC, the March
Report to Congress from various years are used. They can
be found at www.medpac.gov.
For data references provided by the Centers for Medicare
and Medicaid Services (CMS), the FY 2022 Hospice Wage
Index and Quality Reporting Proposed Rule, (CMS-1754-P)
was published in the Federal Register at www.govinfo.gov/
content/pkg/FR-2021-04-14/pdf/2021-07344.pdf on April
14, 2021.
Questions May Be Directed To:
National Hospice and Palliative Care Organization Attention
Email: C[email protected]g
Subject line: Facts and Figures
Phone: 703.837.1500
Web: www.nhpco.org
Email: C[email protected]g
©2021 National Hospice and Palliative Care Organization. All
rights reserved, including the right to reproduce this
publication or portions thereof in any form. Public use of this
report and reported data is authorized if the National
Hospice and Palliative Care Organization is clearly referenced.
Suggested Citation:
2021 Edition: Hospice Facts and Figures. Alexandria, VA:
National Hospice and Palliative Care Organization.
www.nhpco.org/factsigures.
24

NHPCO
1731 King Street
Alexandria, VA 22314
tel. 703.837.1500 | nhpco.org
OCTOBER 2021
