
Journal of the Georgia Public Health Association Journal of the Georgia Public Health Association
Volume 7 Number 2 Article 5
Fall 2019
Health Care Access by Weight Status in the State of Georgia Health Care Access by Weight Status in the State of Georgia
Author A<liations Author A<liations
Elizabeth PullekinesElizabeth Pullekines, Front Street Clinic (Americorps)
Janani Rajbhandari-ThapaJanani Rajbhandari-Thapa, University of Georgia
Corresponding Author Corresponding Author
Janani Rajbhandari-Thapa (jr[email protected])
Follow this and additional works at: https://digitalcommons.georgiasouthern.edu/jgpha
Part of the Public Health Commons
Recommended Citation Recommended Citation
Pullekines, Elizabeth and Rajbhandari-Thapa, Janani (2019) "Health Care Access by Weight Status in the
State of Georgia,"
Journal of the Georgia Public Health Association
: Vol. 7: No. 2, Article 5.
DOI: 10.20429/jgpha.2019.070205
Available at: https://digitalcommons.georgiasouthern.edu/jgpha/vol7/iss2/5
This secondary data analysis is brought to you for free and open access by the Journals at Georgia Southern
Commons. It has been accepted for inclusion in Journal of the Georgia Public Health Association by an authorized
administrator of Georgia Southern Commons. For more information, please contact

Secondary Data Analysis
Health Care Access by Weight Status in the State of Georgia
Elizabeth Pullekines, MPH
1
and Janani Rajbhandari-Thapa, PhD
2
1
Health Outreach Coordinator, Front Street Clinic (Americorps);
2
Department of Health Policy and Management, College of Public Health,
University of Georgia
Corresponding Author: Janani Rajbhandari-Thapa College of Public Health, University of Georgia 211 B Wright Hall (HSC), Athens, GA 30602 706-713-
2700 jrthapa@uga.edu
ABSTRACT
Background: Obesity continues to grow in prevalence in the United States and within the state of Georgia. Obesity is a risk
factor for many chronic and preventable diseases. As such, obese individuals have higher demand for health care services than
non-obese individuals. In addition, the health care system can play a role in preventing obesity and other conditions caused by
obesity.
Methods: This research follows the established positive relationship between health care use and access to health care services
through insurance coverage. The paper analyzes how the Affordable Care Act (ACA) affected insurance coverage and access to
health care services for obese and overweight individuals. A logistic regression was used on data from the Behavioral Risk Factor
Surveillance System.
Results: Results concluded that Georgia residents were less likely to have health insurance after the ACA was passed.
Significant association between weight status and health care services through insurance coverage was not found. The results
show that increased access to care including preventive services for obese and overweight post ACA is yet to be observed.
Conclusions: Findings present a need for lawmakers to develop policy to promote insurance enrollment for Georgian residents.
This is critical as the state sees an increase in overweight and obesity that are risk factor to many chronic disease conditions.
Keywords: Affordable Care Act, obesity, insurance, healthcare
https://doi.org/10.20429/jgpha.2019.070205
INTRODUCTION
Obesity prevalence has been increasing in the United States
(U.S.) since the 1990s. Nearly 38% of adults in the U.S.
were obese in 2014. This increasing trend in adult obesity
rates also applies to southern states. Though Georgia had the
third lowest obesity rate among southern states after Florida
(27.4%) and Virginia (29%), Georgia ranks 20
th
among all
the state in the U.S. in obesity and overweight rate. The
obesity rate in Georgia was 31.4% in 2016. The highest rate
among southern states was West Virginia, with 37.7%
(Centers for Disease Control and Prevention, 2017). Obesity
throughout the nation and the state is pervasive across
gender, ethnic origin, and socioeconomic status with some
variation in trend by race and ethnicity (Flegal et al., 2012).
For adults over the age of 20, men among all races, except
non-Hispanic black, were more likely to be overweight.
Women among all races were more likely to be obese then
men (Ogden et al., 2014). Further, obesity associated
comorbidities have been cited and reported in many
scholarly works (Guh et al., 2009). Obesity has also been
identified as a risk factor for heart disease and cancer, which
are among the top five preventable causes of death (Yoon,
2014). In Georgia, heart and vascular diseases, such as
stroke or hypertension, and some cancers are among the top
ten causes of deaths for adults aged 25 and older (Georgia
Department of Public Health, n.d.).
Furthermore, the cost impact of obesity on the U.S. health
care system is high. Annual cost of obesity was $190 billion
in 2005 (Cawley et al., 2012). In the state of Georgia alone
the direct and indirect costs of obesity was $2 billion in
2003 (Finkelstein et al., 2004). Chronic diseases that obesity
is a risk factor for, such as heart disease and diabetes,
account for $2.3 trillion in health care costs annually in
2008 dollars (Oschman, 2011). Obese individuals’ health
care utilization rates and associated costs was also higher
compared to non-obese individuals (Peterson and
Mahmoudi, 2015). The median increase in mean annual
healthcare costs were 12% for overweight and 36% for
obese individuals, compared to individuals at healthy weight
with highest percentage increase in medications, inpatient
care and ambulatory care (Kent et al., 2017). Furthermore,
studies have found that about 80% of heart disease, stroke,
and type 2 diabetes and 40% of cancers are preventable
(Gerteis et al., 2014). As such understanding factors
associated with prevention and treatment of obesity,
including access to health care, is critical. The focus of this
study is to explore access to health care by weight status.
38
Pullekines and Rajbhandari-Thapa: Health Care Access by Weight Status in the State of Georgia
Published by Georgia Southern Commons, 2019
Health care services can play a role both in obesity
prevention and treatment. To prevent obesity, hospitals may
provide behavioral counseling (Katz and Faridi, 2007).
Hospitals can also engage in outreach activities or have
obesity prevention programs such as skill building classes
for their service area. Healthcare organizations might also
have spaces in their facility for small fitness centers or a
healthful cooking teaching kitchen. This would be an
important step towards addressing obesity as simple
nutrition and weight counseling has been proven to be
effective at reducing weight (McAlpine & Wilson,
2007).While this idea has been considered in the past, there
have been many barriers such as access to care by obese
individuals to seriously offering treatments such as obesity
and nutrition counseling to tackle the obesity issue in the
hospital setting (Kraschnewski et al., 2013; McAlpine &
Wilson, 2007). To treat obesity, health care providers can
utilize more invasive treatment options such as bariatric
surgery (Gloy et al., 2013). Hence it is important to
understand the health care coverage for obese and
overweight individuals.
Utilization of the available obesity prevention and treatment
services depends on obese individuals’ access to health care
through insurance coverage. Health care access and
utilization is dependent on insurance coverage and insurance
coverage measures access to health care. In a study
exploring societal and individual determinants of medical
care insurance coverage was found to affect health care
utilization (Milbank, 2005). In a study, 90% of low-income
uninsured adults stated costs as the main barrier to health
care (Hoffman and Paradise, 2008). Over 40% of uninsured
adults, compared to 18% of insured adults, did not have a
routine checkup in a two-year time frame (Hoffman and
Paradise, 2008). Furthermore, obesity has been found to be
associated with lower socioeconomic status (Newton et al.,
2017). Cost of care is a significant barrier to accessing
health care. As such, utilization of health care is affected by
insurance coverage. Insurance assist individuals in reducing
their health care expenses. Routine checkups are important
to maintain health and avoid long-term health care costs.
Because obesity is an identified risk factor for several
comorbid conditions, access and utilization of health care in
association with weight status is even more critical.
This study aims to analyze how the Affordable Health Care
(ACA) impacted access to health care coverage and health
care coverage by weight status among adults in the state of
Georgia. We hypothesize that those with a higher weight
status would be more likely to obtain health care coverage
and access to health care would have increased post ACA.
Increased access to health care would allow individuals with
more than normal weight to reduce the costs of services that
they receive, regardless of whether it is due specifically to
their weight or a disease associated with excess weight.
METHODS
Data
This study used the state of Georgia’s Behavioral Risk
Factor Surveillance System (BRFSS) data from 2005
through 2015. BRFSS is a telephone-based survey
conducted by the Centers for Disease Control and
Prevention (CDC); the deidentified dataset is made publicly
available on their website at www.cdc.gov
. The survey
collects data on U.S. residents at the state level regarding
resident’s health behavior, chronic health conditions, and
preventative services utilization. Data also includes access
to healthcare, weight status, and metropolitan status. BRFSS
collects responses from participants in all 50 states,
Washington D.C., and territories and provides state
identifiers making studies possible at the state level.
Furthermore, this study was possible as the data set for
Georgia included the same questions regarding the variables
of interest from 2005 to 2015. Further this research does not
constitute Human Subjects Research as per the institution’s
policy as it is based on publicly available deidentified
secondary dataset. The survey question and response option
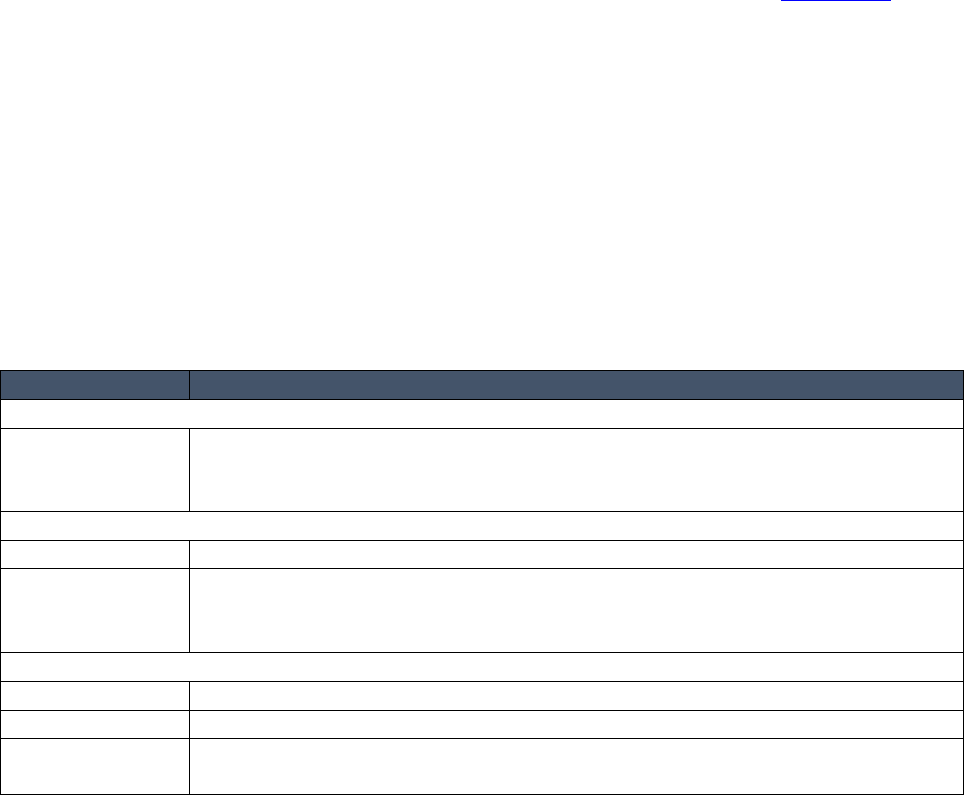
for each variable are shown in Table 1.
Table 1. Data from 2005-2015 BRFSS Surveys
Data
Survey question and response options in BRFSS
Dependent variable
Have insurance
coverage
Do you have any kind of health care coverage, including health insurance,
prepaid plans such as HMOS, or governmental plans such as Medicare, or
Indian Health Service? Yes/ No
Explanatory variables
BMI categories
Underweight or normal (≤ 24.9)/ Overweight (25-29.9)/ Obese (≥30)
Before and after
the Affordable
Care Act
2005-2015 (1 if 2005 through March 2010, 0 if April 2010 through 2015)
Confounding variables
Gender
Male/ Female
Age
18-24/ 25-34/ 35-44/ 45-54/ 55-645/ 65 and above
Race
White/ Black/ American Indian or Alaskan Native (Native)/ Asian/ Native
Hawaiian or Pacific Islander (Hawaiian) / Other race
39
Journal of the Georgia Public Health Association, Vol. 7, No. 2 [2019], Art. 5
https://digitalcommons.georgiasouthern.edu/jgpha/vol7/iss2/5
DOI: 10.20429/jgpha.2019.070205

Data
Survey question and response options in BRFSS
Income
Less than $15,000/ $15,000 to $24,999/ $25,000 to $34,999/ $35,000 to
$49,999 /$50,000 or more
Education
Did not graduate high school/ Graduated high school/ Attended college or
technical school/ Graduated from College or Technical School
Metropolitan
status (MSA)
In the center city of an MSA/ Outside the center city of an MSA, but inside
the county containing the center city/ Inside a suburban county of the MSA/
In a MSA that has no city center/ Not in an MSA
Employment
status
Employed for wages/ Self-employed/ Out of work for 1+ year/ Out of work
for less than 1 year/ A homemaker/ A student/ Retired/ Unable to work
General health
Would you say that in general, your health is?
Excellent/ Very Good/Good/Fair/Poor
Have poor
physical health
Now thinking about your physical health, which includes physical illness and
injury, for how many days during the past 30 days was your physical health
not good? # of days/ None
Have poor
mental health
Now thinking about your mental health, which includes stress, depression,
and problems with emotions, for how many days during the past 30 days was
your mental health not good? # of days/ None
Poor health
preventing usual
activities
During the past 30 days, for about how many days did poor physical health or
mental health keep you from doing your usual activities, such as self-care,
work, or recreation? # of days/ None
Checkup
About how long has it been since you last visited a doctor for a routine
checkup? Within past year/ Within past 2 years/ Within past 5 years/ 5 or
more years ago/ Never
Unable to
receive care due
to cost
About how long has it been since you last visited a doctor for a routine
checkup? [A routine checkup is a general physical exam, not an exam for a
specific injury, illness, or condition.]
This study assessed access to health care by weight status in
Georgia using insurance coverage as a proxy to health care
access, which affects utilization of obesity prevention and
treatment-oriented health care services. Data from the 2005
to 2015 Behavioral Risk Factor Surveillance System
surveys were compiled to create a time series data and
logistic regression analysis was used. This study tested if
obese and overweight individuals have a higher likelihood
of having insurance coverage given the established
relationship between higher weight status and chronic
diseases. The model was controlled for confounding from
socio-demographic variables such as age, income,
education, employment status, and race along with
metropolitan status. Further, prior to 2010, most states
allowed insurance companies in the individual market to
deny individuals’ health insurance coverage based on health
status and allowed rates to be set based on health status (Lee
et al., 2010). Obesity was identified as a risk factor for
several disease as early as the 1990s (Must et al., 1999). As
a result, obese individuals may have been denied health
insurance services due to health conditions that list obesity
as a risk factor. The enactment of the Affordable Care Act
(ACA) in 2010, prohibited insurance companies from
denying individuals coverage due to pre-existing conditions.
The study accounts for the post ACA period due to its
potential impact on insurance coverage. Period after ACA is
also important to identify because post ACA individuals
with insurance coverage would have increased access to
preventive health care such as annual wellness check. This
is important with respect to obesity and it could potentially
help identify weight issues earlier rather than later when it
has caused other health problems or treatment are costlier.
Data analysis
Data from each year from 2005 to 2015 were downloaded
and compiled to develop a time series data. Pregnant women
were excluded from the study. Variables were adjusted to
accommodate variations in answers to the same questions in
different years. For example, the years 2011-2015 had four
categories for BMI (underweight, normal, overweight, and
obese), while 2005-2010 only used three. Underweight and
normal weight in 2011-2015 were combined to match data
from previous years. A logistic regression model was used
to predict insurance coverage as a proxy to health care
access by weight status and enactment of the Affordable
Care Act. As such, having any health care coverage served
as the dependent variable. This was measured by the
responses to the question “Do you have any kind of health
care coverage, including health insurance, prepaid plans
such as HMOs, or governmental plans such as Medicare or
Indian Health Service?” The explanatory variables of
interest included year and weight status. Year variable was
40
Pullekines and Rajbhandari-Thapa: Health Care Access by Weight Status in the State of Georgia
Published by Georgia Southern Commons, 2019

dichotomized to before and after the Affordable Care Act
was passed. Prior to the Affordable Care Act ranged from
2005 to March 2010. After the Affordable Care ranged from
April 2010 to 2015. This was due to the ACA being signed
into law on March 23, 2010 (“H.R. 3590-11
th
Congress”,
2010). The dataset is rich and allowed adjustment for
confounding from sociodemographic variables such as
gender, age, race, income, and education. In addition, the
model controlled for other potential confounders such as
employment status, geographical location (metropolitan
status), general, physical and mental health, and the state of
being in poor health. Education may influence knowledge of
what kind of coverage is available. Employment status can
influence where individuals receive health insurance and the
type of coverage they receive. Metropolitan status (MSA)
can influence the number of insurance providers individuals
have access to. For example, there may be more providers in
a city center than a rural community. The data were
analyzed using STATA version 14.2.
RESULTS
The demographics of the overall sample and the insured and
uninsured categories within this sample is shown in Table 2.
The highest proportion of respondents in each category were
white followed by African-American. The insured
population had a slightly higher percentage (71%) of white
individuals and slightly lower percentage of African-
American respondents (22%) compared to 63% and 28%
within the uninsured category. About 36% of the overall
population had a college degree followed by high school or
some college education. The percentage of college
graduates within the insured was highest (36%), while the
percentage of high school graduates was highest (35%)
within uninsured category. Proportion of male respondents
were higher than female. Most individuals in all three
populations were between the ages of 35 and 44. About 32%
of the respondents in all categories were from a suburban
county. Highest proportion (35%) of the uninsured lived
outside an MSA. Highest proportion (43%) of respondents
in the insured category had an income above $50,000. Only
20% of the uninsured population had an income over
$50,000. For the uninsured population, having an income
between $15,000 and $24,999 made up the largest
percentage, at about 32%. In terms of employment,
employed for wages make up the largest percentage for all
three categories.
Table 2. Respondent’s demographics (%)
Overall
n=12,437
Insured
n=10,855
Uninsured
n=1,582
Race
White
70
71
63
Black
23
22
28
Hispanic
3
3
4
Asian
1
1
1
American Indian
1
1
1
Other Race
1
1
1
Multiracial
1
1
2
Education
< High school
11
10
18
High school graduate
27
25
35
Some college
27
26
27
College graduate
36
39
20
Gender
Male
54
54
58
Female
46
46
42
Age
18-24
5
4
9
25-34
17
16
22
35-44
27
26
30
45-54
14
13
18
55-64
17
17
18
≥ 65
20
23
3
Metropolitan status
Not in MSA
29
28
35
MSA suburban county
32
32
31
MSA county
12
13
11
MSA city center
26
27
23
Income
< $15,000
13
11
24
41
Journal of the Georgia Public Health Association, Vol. 7, No. 2 [2019], Art. 5
https://digitalcommons.georgiasouthern.edu/jgpha/vol7/iss2/5
DOI: 10.20429/jgpha.2019.070205

Overall
n=12,437
Insured
n=10,855
Uninsured
n=1,582
$15,000-24,999
19
17
32
$25,000-34,999
12
12
13
$35,000-49,999
14
15
11
≥ $50000
43
46
20
Employment status
Employed for wages
46
47
40
Self-employed
8
7
13
No work > 1 year
3
2
11
No work < 1 year
3
2
7
Homemaker
6
6
6
Student
3
2
4
Unable to work
12
11
13
Retired
20
22
5
Year
Before ACA (Jan 2005-Mar 2010)
55
55
57
After ACA (Apr 2010-Dec 2015)
45
45
43
Table 3 shows the demographics of respondents by weight
status. Most of the respondents in each of the three
categories reported being white, followed by African-
American. In terms of education, most overweight and
normal or underweight respondents reported having a
college degree, while most obese respondents reported
having a high school degree. About 49% of obese
respondents reported after the Affordable Care Act was
passed. This was higher than overweight and normal or
underweight. Obese and overweight individuals were more
likely to report being male, 54% and 63%, respectively.
About 55% of normal or underweight individuals reported
being female. Most respondents in each category reported to
be between the ages of 35 and 44. About 32% of obese,
33% of overweight, and 31% of normal or underweight
reported living in a suburban county of a metropolitan city.
Most individuals in each weight status reported having an
income of over $50,000. Nearly 45-50% of respondents in
each weight category reported to be employed for wages.
About 16% of obese reported being unable to work. This
was about twice the percentage for each of the other two
weight status.
Table 3. Respondents’ demographics by weight status (%)
Obese
(n=4,186)
Overweight
(n= 4,367)
Normal
(n=3,884)
Race
White
65
73
74
Black
30
21
18
Hispanic
3
2
3
Asian
0
1
2
American Indian
1
1
1
Other Race
1
1
1
Multiracial
1
1
1
Education
< High school
12
10
10
High school graduate
30
26
23
Some college
28
26
25
College graduate
30
38
42
Gender
Male
54
63
45
Female
46
37
55
Age
18-24
3
3
9
25-34
15
16
21
35-44
27
25
29
42
Pullekines and Rajbhandari-Thapa: Health Care Access by Weight Status in the State of Georgia
Published by Georgia Southern Commons, 2019

Obese
(n=4,186)
Overweight
(n= 4,367)
Normal
(n=3,884)
45-54
17
15
10
55-64
20
19
12
≥ 65
19
23
19
Metropolitan Status
Not in MSA
32
29
26
MSA suburban county
32
33
31
MSA county
11
13
13
MSA city center
24
25
29
Income
< $15,000
15
10
12
$15,000-24,999
21
18
18
$25,000-34,999
12
12
11
$35,000-49,999
14
14
14
≥ $50000
37
46
45
Employment Status
Employed for wages
45
47
45
Self-employed
7
8
9
No work > 1 Year
4
3
4
No work < 1 Year
3
3
3
Homemaker
4
5
8
Student
2
2
4
Unable to work
16
10
9
Retired
19
23
19
Year
Before ACA (Jan 2005-Mar 2010)
51
56
59
After ACA (Apr 2010-Dec 2015)
49
44
41
Table 4 shows the health status of respondents. Most
respondents in the overall (34%) and insured categories
(33%) were overweight. For the uninsured population, obese
individuals had the highest percentage (36%). About 87% of
the overall population reported having insurance. Finally,
most individuals reported having a checkup within the past
year. Most respondents reported being in good health across
all categories. About 71% of the overall and insured
population and 68% of the uninsured population reported
having poor physical health in the last 30 days. About 62%
of the overall population and 60% of the insured reported
having poor mental health in the past 30 days. Seventy one
percent of the uninsured respondents reported poor mental
health.
Table 4. Respondents’ health status (%)
Overall
n=12,437
Insured
n=10,855
Uninsured
n=1,582
Weight status
Obese
33.66
33.29
36.16
Overweight
35.11
35.63
31.54
Normal
31.23
31.07
32.3
Have insurance coverage
87.28
100
0
Unable to receive care due to cost
20.95
16.55
51.14
Time Since Last Checkup
Never
0.97
0.81
2.09
Within the past year
74.41
77.52
53.03
Within 2 years
11.06
10.58
14.41
Within 5 years
6.65
5.73
12.96
5 or more years
6.91
5.36
17.51
43
Journal of the Georgia Public Health Association, Vol. 7, No. 2 [2019], Art. 5
https://digitalcommons.georgiasouthern.edu/jgpha/vol7/iss2/5
DOI: 10.20429/jgpha.2019.070205

Overall
n=12,437
Insured
n=10,855
Uninsured
n=1,582
General health
Excellent
12.14
12.42
10.24
Very good
28.83
29.33
25.41
Good
30.19
29.96
31.8
Fair
18.37
17.84
22
Poor
10.46
10.45
10.56
Have poor physical health
71.02
71.52
67.64
Have poor mental health
61.71
60.34
71.11
Poor health preventing usual activities
41.61
41.02
45.64
Table 5 shows the respondents’ health status by weight.
Overweight respondents had the highest percentage (89%)
of being insured followed by obese (86%) and normal or
underweight (87%). About 26% of obese individuals
reported they were unable to receive care due to costs. All
three weight categories mostly reported having had a
checkup within the past year. Obese had the highest
percentage while normal or underweight had the lowest. In
terms of general health, about 35% of obese respondents
reported being in good health. About 31% of overweight
and 33% of normal or underweight individuals reported
their health as very good. A higher percentage of obese
individuals reported their health as being fair or poor than
the other two weight categories. Obese were also less likely
to report their general health as being excellent. About 77%
of obese individuals reported having poor physical health in
the past month. Normal or underweight respondents were
the most likely to reported having poor mental health in the
past month. Finally, about 47% of obese reported having
poor health preventing them from engaging in their usual
activities.
Table 5. Respondents’ health status by weight (%)
Obese
(n=4,186)
Overweight
(n= 4,367)
Normal
(n=3,884)
Have insurance coverage
86.34
88.57
86.84
Unable to receive care due to cost
25.9
17.66
19.31
Time Since Last Checkup
Never
0.72
1.03
1.18
Within the past year
77.16
73.87
72.04
Within 2 years
9.82
11.15
12.31
Within 5 years
6.24
7.01
6.69
5 or more years
6.07
6.94
7.78
General health
Excellent
5.47
12.18
19.28
Very good
22.17
31.3
33.24
Good
34.5
30
25.77
Fair
24.7
16.78
13.34
Poor
13.16
9.73
8.37
Have poor physical health
76.59
70.74
65.35
Have poor mental health
61.47
59.45
64.52
Poor health preventing usual
activities
47.37 38.68 38.7
The results of the logistic regression are shown in Table 6,
reported are the odds ratio for having insurance coverage by
weight status, and before and after ACA with controls for
potential confounding from gender, education level, income
level, employment status, age, metropolitan status, race,
checkup, unable to receive care due to cost, general health,
have poor physical health, have poor mental health, and
poor health preventing usual activities. No significant
44
Pullekines and Rajbhandari-Thapa: Health Care Access by Weight Status in the State of Georgia
Published by Georgia Southern Commons, 2019

differences were seen in the likelihood of having insurance
plan by weight status. Finally, after the Affordable Care Act
was passed, Georgians were 21% less likely to have
insurance (p<0.01). Confounding from race was not
significant for any race category. However, there were
significant confounding from education status. Those with
less than high school education were 41% less likely to have
health insurance than college graduates (p<0.001) followed
by high school graduate (32% less likely, p<0.001) and
some college (21% less likely, p<0.001). Males were 53%
less likely to have health insurance than females (p<0.001).
Each age category under the age of 65 were at least 81%
less likely to have insurance than those over 65 (p<0.001).
Those between 18 and 25 were the least likely (89%,
p<0.001) to have insurance coverage. Likelihood of having
insurance increased with age. Individuals living outside of
the MSA were 17% less likely to have insurance than those
within a city center (p=0.026). Income revealed similar
trends to age, higher the income more likely an individual
would be insured. Those with an income less than $15,000
were 73% less likely (p<0.001) than those with an income
higher than $50,000 to have insurance. Regarding
employment, those employed for wage were 37% less likely
to have insurance (p=0.003). Students were 48% less likely
to have insurance than retired (p=0.003). Homemakers and
those with no work for less than one year were just under
45% less likely to have insurance (p<0.001). Self-employed
and those without work for over a year were 71% and 74%,
respectively, less likely to have insurance than the retired
population (p<0.001). Individuals unable to receive care due
to cost were 43% less likely to have insurance (p<0.001).
Those who have had a longer time since their last checkup
were less likely to have insurance (p<0.001). The other
health related measures were not significant.
Table 6. Odds ratio from logistic regression
Odds ratio
p value
95% CI
BMI
Obese
1.05
0.564
0.90-1.21
Overweight
1.12
0.125
0.97-1.31
Normal or underweight
1.00
Year
After ACA
0.79
<0.001
0.69-0.89
Before ACA
1.00
Education
< High school
0.59
<0.001
0.48-0.74
High school graduate
0.68
<0.001
0.57-0.81
Some college
0.79
0.007
0.66-0.94
College graduate
1.00
Gender
Male
0.47
<0.001
0.41-0.55
Female
1.00
Age
18-24
0.11
<0.001
0.07-0.16
25-34
0.14
<0.001
0.09-0.20
35-44
0.14
<0.001
0.10-0.20
45-54
0.18
<0.001
0.13-0.25
55-64
0.19
<0.001
0.13-0.26
≥ 65
1.00
Metropolitan status
Not in MSA
0.83
0.026
0.71-0.98
MSA suburban county
0.88
0.112
0.75-1.03
MSA county
0.97
0.795
0.78-1.20
MSA city center
1.00
Income
< $15,000
0.27
<0.001
0.22-0.34
$15,000-24,999
0.32
<0.001
0.27-0.39
$25,000-34,999
0.50
<0.001
0.40-0.62
$35,000-49,999
0.66
<0.001
0.54-0.81
≥ $50,000
1.00
Employment status
45
Journal of the Georgia Public Health Association, Vol. 7, No. 2 [2019], Art. 5
https://digitalcommons.georgiasouthern.edu/jgpha/vol7/iss2/5
DOI: 10.20429/jgpha.2019.070205

Odds ratio
p value
95% CI
Employed for wages
0.63
0.003
0.46-0.85
Self-employed
0.29
<0.001
0.21-0.40
No work > 1 Year
0.26
<0.001
0.18-0.37
No work < 1 Year
0.36
<0.001
0.25-0.52
Homemaker
0.38
<0.001
0.26-0.56
Student
0.52
0.003
0.34-0.81
Retired
1.00
Health
Unable to receive care due to cost
0.37
<0.001
0.33-0.42
Time Since last checkup
0.76
<0.001
0.72-0.81
Race had no significant confounding effect, hence not reported in the table.
DISCUSSION
This study examines access to health care by weight status
in the state of Georgia using insurance coverage as a proxy
to health care access and thus utilization of obesity
prevention and treatment-oriented health care services.
Findings suggest that obese and overweight residents did
not have a higher likelihood of having insurance coverage
compared to non-obese individuals. The direction of the
coefficients was as expected, but not significant. Further,
Georgia residents were less likely to be insured after the
Affordable Care Act was passed. This was not entirely
expected due to the individual mandate outlined by the
reform law. This result was different from another study that
found that there was a 27.4% decrease in uninsured rates
between 2010 and 2015. This study found larger decreases
in uninsured rates for the three southern states that expanded
Medicaid in 2014 than those that did not (Garret. &
Gangopadhyaya, 2016). However, this study did not look at
weight status. These differences could be attributed to
Georgia lawmakers not expanding Medicaid. Several
Georgians may have fallen in the coverage gap and were
unable to afford insurance coverage. Living outside of an
MSA may have influenced this association, as nearly 30%
of respondents lived outside these areas. This population
was the second largest of the overall respondents. This
region was the only area that had a statistically significant
association with having less insurance than those living in a
city center. Such, rural urban gap in health care safety net
program has also been previously documented in the state of
Georgia (Minyard et al., 2016).
Obesity has been found to be associated with certain
socioeconomic status (SES). One meta-analysis found that
overall, those with lower SES were more likely to be obese
(Newton et al., 2017). Though there are individual variation,
there is a predictable pattern. Studies have found that those
with higher incomes and higher education levels were more
likely to be insured (Swinburn, 2011 and Hong et al., 2016).
This is consistent with our findings. This could be because
those with higher incomes may find insurance more
affordable and would be more willing to purchase it. Several
factors can influence the relationship between education and
insurance status. Educated adults are less likely to be
unemployed, as well as have higher incomes. More
educated individuals may have the knowledge or social
networks to help navigate healthcare more easily. They may
also live in areas where insurance is more accessible than
less educated individuals (Zimmerman et al., 2015). Males
having less insurance is consistent with other research (Day
et al., 2015; Long et al., 2011; Hong et al., 2016; Dahlen,
2015). Each study reported similar numbers and that the
percentage of men and women having insurance grew closer
after the ACA was passed. Similar percentages of men and
women having Medicare and private insurance were found
(Day et al., 2015).
The findings of this study have policy implications at the
state level. Obese and overweight individuals of Georgia not
having a higher likelihood of having insurance coverage is
concerning. It is further concerning that there was decrease
in insurance coverage after the Affordable Care Act. Health
insurance can help reduce the costs of health care services
for patients, including obese patients who are at a higher
risk for diseased condition. This would especially be
beneficial for lower income individuals who were found to
be less likely to have insurance. Therefore, Georgia
lawmakers should consider expanding Medicaid. Efforts
also should be made to increase the insurance rates for those
who would qualify for employer-sponsored or Marketplace
based plans as well. This could increase the number of
individuals, including obese and overweight individuals,
with health insurance, as well as the number of individuals
who have access to healthcare. Special attention is also
needed to increase insurance coverage among individuals
with obesity and overweight in future policies developed to
promote insurance coverage.
In addition to increasing the number of insured individuals,
expansion of insurance coverage, specifically to low income
population through Medicaid can positively influence
economic activity and employment rates at the state level.
One report noted that 70,343 jobs could be created statewide
in Georgia because of Medicaid expansion, mostly in the
healthcare sector. Real estate, food services, transit and
ground passenger transportation, employment services,
wholesale trade businesses, and construction would also see
an increase in employment. Yearly economic output would
increase by an average of $8.2 billion because of these new
jobs. State and local tax revenue would be increased by an
average of $276.5 million, annually (Custer, 2013).
Another report noted that an investment of 1% of the state
46
Pullekines and Rajbhandari-Thapa: Health Care Access by Weight Status in the State of Georgia
Published by Georgia Southern Commons, 2019

budget could create $65 billion in new economic activity
over 10 years, as well as create over 56,000 jobs throughout
Georgia. State and local tax revenue would increase by $2.2
billion over the same 10-year period (Sweeney, 2013).
CONCLUSIONS
This study aimed to look at the association between weight
status and insurance coverage among Georgia residents and
how the ACA influenced this association. Results
concluded that obese and overweight residents in the state of
Georgia did not have a higher likelihood of having
insurance coverage compared to non-obese individuals. This
conclusion is concerning as the literature is well established
that obese and overweight individuals are at a higher risk for
several preventable chronic disease conditions. Further,
having access to healthcare is crucial to this population for
obesity prevention and treatment. Suggested that Georgia
residents were less likely to have health insurance after the
ACA was passed. This study demonstrates the need to
promote insurance for Georgia residents.
Acknowledgements
There was no funding for this data.
Statement of Student-Mentor Relationship: The lead author for
this report is Elizabeth Pullekines, a Master of Public Health
student in the Department of Health Policy and Management,
College of Public Health, University of Georgia. Dr. Janani
Rajbhandari-Thapa, the senior author, served as her mentor.
References
Cawley J, Meyerhoefer C. The medical care costs of obesity: an
instrumental variables approach. J Health Econ. 2012;
31(1):219-230. Doi: 10.1016/j.jealeco.2011.10.003.
Centers for Disease Control and Prevention. (2017). BRFSS
Prevalence & Trends Data. Retrieved from
https://www.cdc.gov/brfss/brfssprevalence/index.html
.
Custer, W.S. (2013, February). The Economic Impact of Medicaid
Expansion in Georgia.
Healthcare Georgia Foundation. Retrieved from
http://www.healthcaregeorgia.org/uploads/file/Georgia_Medicai
d_Economic_Impact.pdf.
Dahlen, H.M. (2015). “Aging Out” of Dependent Coverage and the
Effects on US Labor Market And Health Insurance Choices.
American Journal of Public Health, Supplement 105(55), S640-
S650.
Day, J.C., O’Hara, B., Taylor, D. (2015, September 16). Another
Difference Between the Sexes-Health Insurance Coverage: Men
Lag Behind Women in Health Insurance Coverage.
Census.
http://blogs.census.gov/2015/09/16/another-difference-
between-the-sexes-health -insurance-coverage-3/.
Finkelstein, E.A., Fiebelkorn, I.C., Wang, G. (2004). State-Level
Estimates of Annual Medical Expenditures Attributable to
Obesity. Obesity Research, 12(1), 18-24. Doi:
10.1038/oby.2004.4.
Flegal, K.M., Carroll, M.D., Kit, B.K., Ogden, C.L. (2012,
February 1). Prevalence of obesity And trends in the distribution
of body mass index among US adults, 1999-2010. JAMA,
307(5), 491-7. Doi: 10.1001/jama.2012.39.
Georgia Department of Public Health. Community Health Needs
Assessment Dashboard. Online Analytical Statistical
Information System. Retrieved from
https://oasis.state.ga.us/CHNADashboard/Default.aspx
Garrett, B., Gangopadhyaya, A. (2016, December). Who Gained
Health Insurance Coverage Under the ACA, and Where Do
They Live? The Urban Institute. Retrieved from
https://www.urban.org/sites/default/files/publication/86761/2001
041-who-gained-health-insurance-coverage-under-the-aca-and-
where-do-they-live.pdf
Gerteis, J., Izrael, D., Deitz, D., LeRoy, L., Ricciardi, R., Miller,
T., Basu, J. (2014, April). Multiple Chronic Conditions
Chartbook. Agency for Healthcare Research and Quality.
Retrieved from
https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/
prevention-chronic- care/decision/mcc/mccchartbook.pdf.
Gloy, V., Briel, M., Bhatt, D.L., Kashyap, S.R., Mingronge, G.,
Bucher, H.C., Nordmann, A.J.
(2013, October 22). Bariatric surgery versus non-surgical
treatment for obesity: a
Systematic review and meta-analysis of randomized controlled
trials. BMJ. Doi:
https://doi.org/10.1136/bmj.f5934.
Guh, D.P., Zhang, W., Bansback, N., Amarsi, Z., Birmingham,
C.L., Anis, A.H. (2009, March 25). The incidence of co-
morbidities related to obesity and overweight: A systematic
Review and meta-analysis. BMC Public Health. Doi:
https://doi.org/10.1186/1471-2458
-9-88.
Hoffman, C., Paradise, J. (2008, June). Health Insurance and
Access to Health Care in the United
States. Annals of the New York Academy of Sciences. Doi:
10.1196/annals.1424.00
Hong, Y.R., Holcom, D., Bhandari, M., Larkin, L, (2016).
Affordable care act: comparison of Healthcare indicators among
different insurance beneficiaries with new coverage
Eligibility. BMC Health. Doi: 10.1186/s12913-016-1362-1.act.
H.R. 3590-111
th
Congress: Patient Protection and Affordable Care.
(2010). Retrieved from
https://govtrack.us/congress/bills/111/hr3590.
Kraschnewski, J. L., Sciamanna, C. N., Stuckey, H. L., Chuang, C.
H., Lehman, E. B., Hwang, K. O., . . . Nembhard, H. B. (2013).
A silent response to the obesity epidemic: decline in US
physician weight counseling. Med Care, 51(2), 186-192.
doi:10.1097/MLR.0b013e3182726c33
Katz, D.L., Faridi, Z. (2007). Health Care System Approaches to
Obesity Prevention and Control. In Kumanyika, S.,
Brownson, R.C. (Eds.), Handbook of Obesity Prevention: A
Resource for Health Professionals (285-316). New York, NY:
Springer Science + Business Media, LLC.
Kent, S., Fusco, F., Gray, A., Jebb, S.A., Cairns, B.J., &
Mihaylova, B. (2017, May 22). Body Mass index and healthcare
costs: a systematic literature review of individual participant
Data studies. Obesity Reviews. Doi: 10.1111/obr.12560.
Lee, J.S., Sheer, J.L.O., Lopez, N., & Rosenbaum, S. (2010, July-
August). Coverage of Obesity Treatment: A State-by-State
Analysis of Medicaid and State Insurance Law. Public
Health Report, 125(4): 596-604. Retrieved from
https://www.ncbi.nlm.nigh.gov/pmc/articles/PMC288611/
.
Long, S.K., Stockley, K., Shulman, S. (2011). How Gender Gaps
in Insurance Coverage Access to Care Narrowed under Health
Reform? Findings from Massachusetts. American
Economic Review: Papers & Proceedings, 101(3), 640-644.
Doi: 10.1257/aer.101.3640.
McAlpine, D. D., & Wilson, A. R. (2007). Trends in obesity-
related counseling in primary care: 1995-2004. Med Care, 45(4),
322-329. doi:10.1097/01.mlr.0000254575.19543.01
Milbank, Q. (2005, December). Societal and Individual
Determinants of Medical Care Utilization in the United States.
The Milbank Quarterly. Doi: 10.1111/j.1469-
0009.2005.00428.x.
47
Journal of the Georgia Public Health Association, Vol. 7, No. 2 [2019], Art. 5
https://digitalcommons.georgiasouthern.edu/jgpha/vol7/iss2/5
DOI: 10.20429/jgpha.2019.070205

Minyard, K., Parker, C., Butts, J. (2016). Improving rural access to
care: Recommendations for Georgia’s health care safety net.
Journal of Georgia Public Health Association, 5(4), 387-396.
Retrieved from
https://www.gapha.org/wp-content/uploads/2016/06/14-5.412-
Improving-rural-access-to care.pdf.
Must, A., Spadano, J., Coakley, E.H., Field, A.L., Colditz, G. &
Dietz W.H. (1999, October 27). The Disease Burden
Associated With Overweight and Obesity. The JAMA Network.
Retrieved from
http://jamanetwork.com/journals/jama/fullarticle/192030
Newton, S., Braithwaite, D., Akinyemiju, T.F., Xiao, G. (Ed.)
(2017, May 16). Socio-economic status over the Life course
and obesity: Systematic review and meta-analysis. PLoS One,
12(5). Doi: 10.1371/journal.pone.0177151.
Ogden CL, Carroll MD, Kit BK, Flegal KM. (2014). Prevalence of
childhood and adult obesity in the United States, 2011-2012.
JAMA. 311(8):806-814. Doi: 10.1001/jama.2014.732
Oschman, J.L. (2011, April). Chronic Disease: Are We Missing
Something? Journal of Alternative Complementary Medicine,
17(4): 283-285. Doi: 10.1089/acm.2011.0101.
Peterson, M.D., Mahmoudi, E. (2015). Healthcare Utilization
Associated with Obesity and Physical Disabilities. American
Journal of Preventative Medicine, 48(4): 426-435.
Doi:10.1016/j.amepre.2014.11.007
.
Sweeney, T. (2013, February). The Dollars and Sense of
Expanding Medicaid in Georgia: Medicaid Expansion Yields
Great Return for Georgia’s Economy. Georgia Budget
& Policy Institute. Retrieved from
https://gbpi.org/wp-content/uploads/2013/02/Cover-Georgia1.pdf.
Swinburn, B.A., Sacks, G., Hall, K.D., McPherson, K., Finegood,
D.T., Moodie, M.L., Gortmaker, S.L. (2011, August 27). The
global obesity pandemic: shaped by global
Drivers and local environments. Lancet, 378(9793), 804-14.
Doi: 10.1016/S0140-6736(11)60813-1.
Yoon, P.W., Bastian, B., Anderson, R.N., Collins, J.L., Jaffe,
H.W., & Centers for Disease Control and Prevention (CDC).
(2014, May 2). Potentially preventable deaths from the five
leading Causes of death – United States, 2008-2010. Morbidity
and Mortality Weekly Report, 63(17), 369-74. Retrieved from
https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6317a1.ht.
Zimmerman, E.B., Woolf, S.H., Haley, A. (2015, September).
Population Health: Behavioral and Social Science Insights:
Understanding the Relationship between Education and Health.
Agency for Healthcare Research and Quality. Retrieved from
https://www.ahrq.gov/professionals/education/curriculum-
tools/population health/zimmerman.html.
© Elizabeth Pullekines, and Janani Rajbhandari-Thapa. Originally published in jGPHA (http://www.gapha.org/jgpha/) October 25, 2019. This is
an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No-Derivatives License
(http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the
original work ("first published in the Journal of the Georgia Public Health Association…") is properly cited with original URL and bibliographic
citation information. The complete bibliographic information, a link to the original publication on http://www.gapha.jgpha.org/, as well as this
copyright and license information must be included.
48
Pullekines and Rajbhandari-Thapa: Health Care Access by Weight Status in the State of Georgia
Published by Georgia Southern Commons, 2019
